| Outcome | RCT | Neuraxial | General | GRADE* | Effect | Estimate (95% CI) |
|---|---|---|---|---|---|---|
| N (Total) | N (Total) | |||||
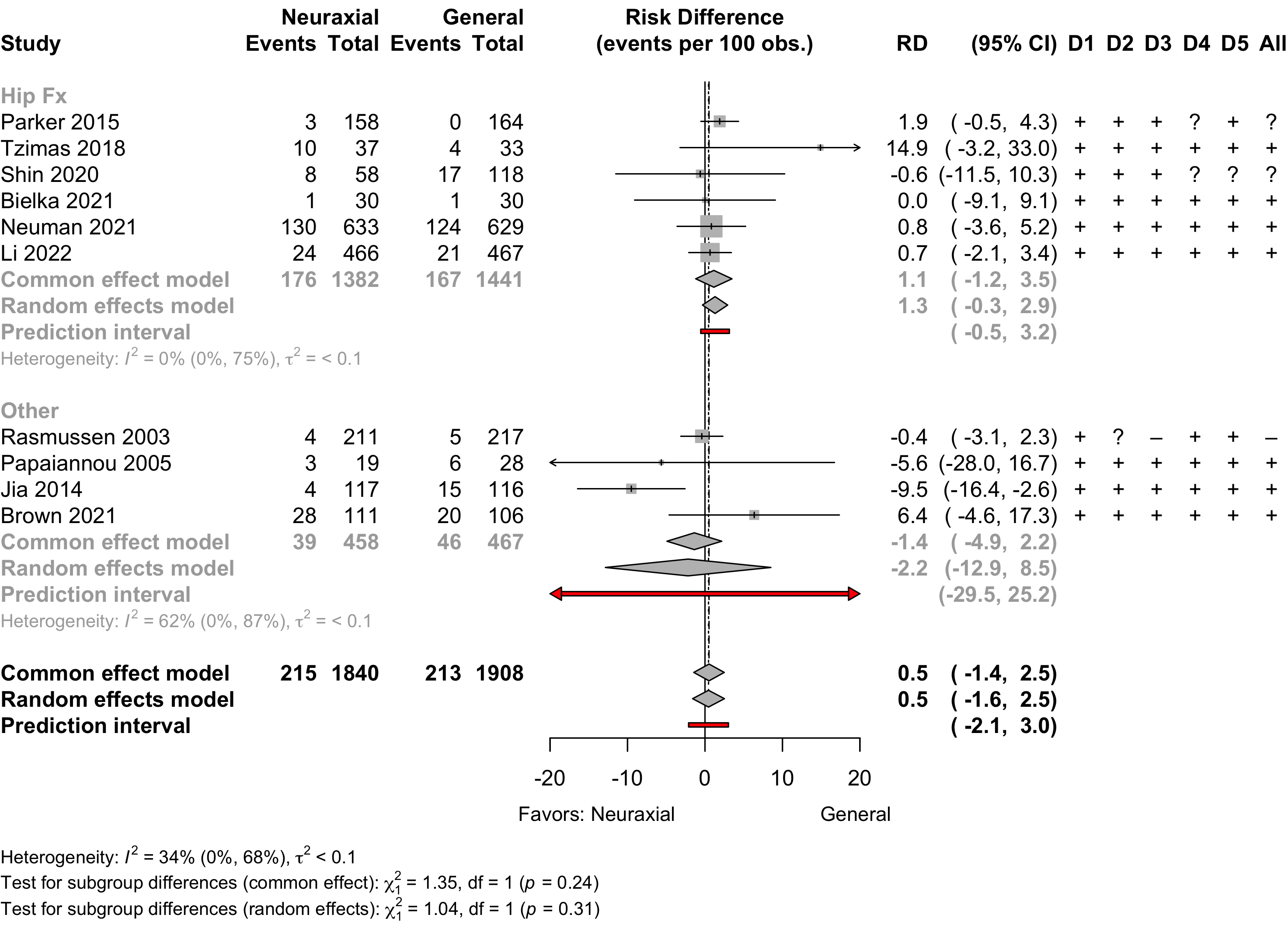
| Delirium | 10 | 215 (1,840) | 213 (1,908) | RR | 1.06 (0.84–1.33)†,‡ | |
| Neurocognitive disorder <30 days | 4 | 78 (336) | 88 (355) | RR | 0.91 (0.56–1.48) | |
| Neurocognitive disorder 30 days to 1 yr | 1 | 23 (176) | 25 (188) | RR | 0.98 (0.58–1.67) | |
| Physical function | 3 | (355) | (371) | SMD | 0.01 (-0.39 to 0.42)§ | |
| Complications** | 13 | see below | ||||
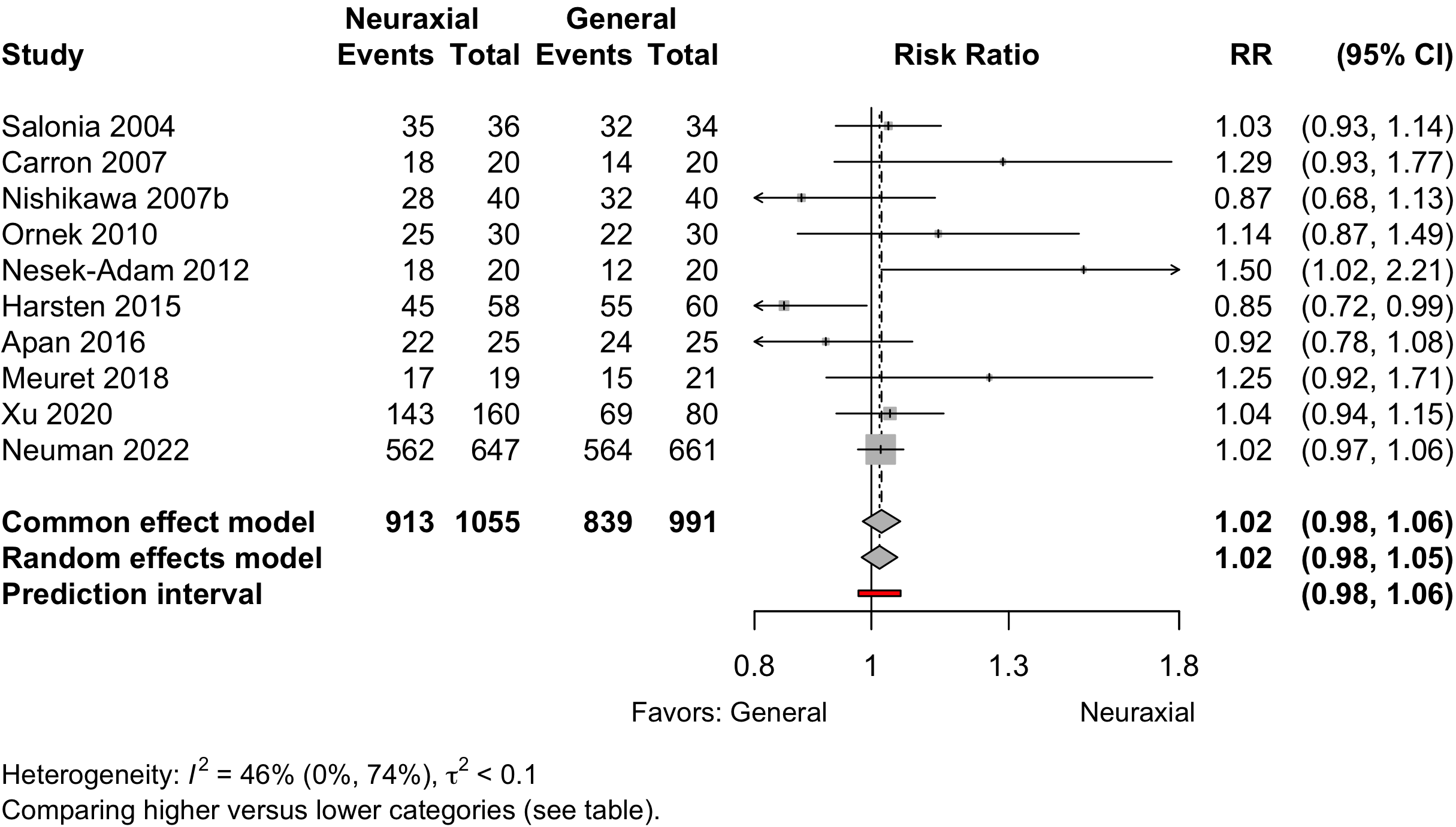
| Patient satisfaction | 10 | 913 (1,055) | 839 (991) | RR | 1.02 (0.98–1.05)†† | |
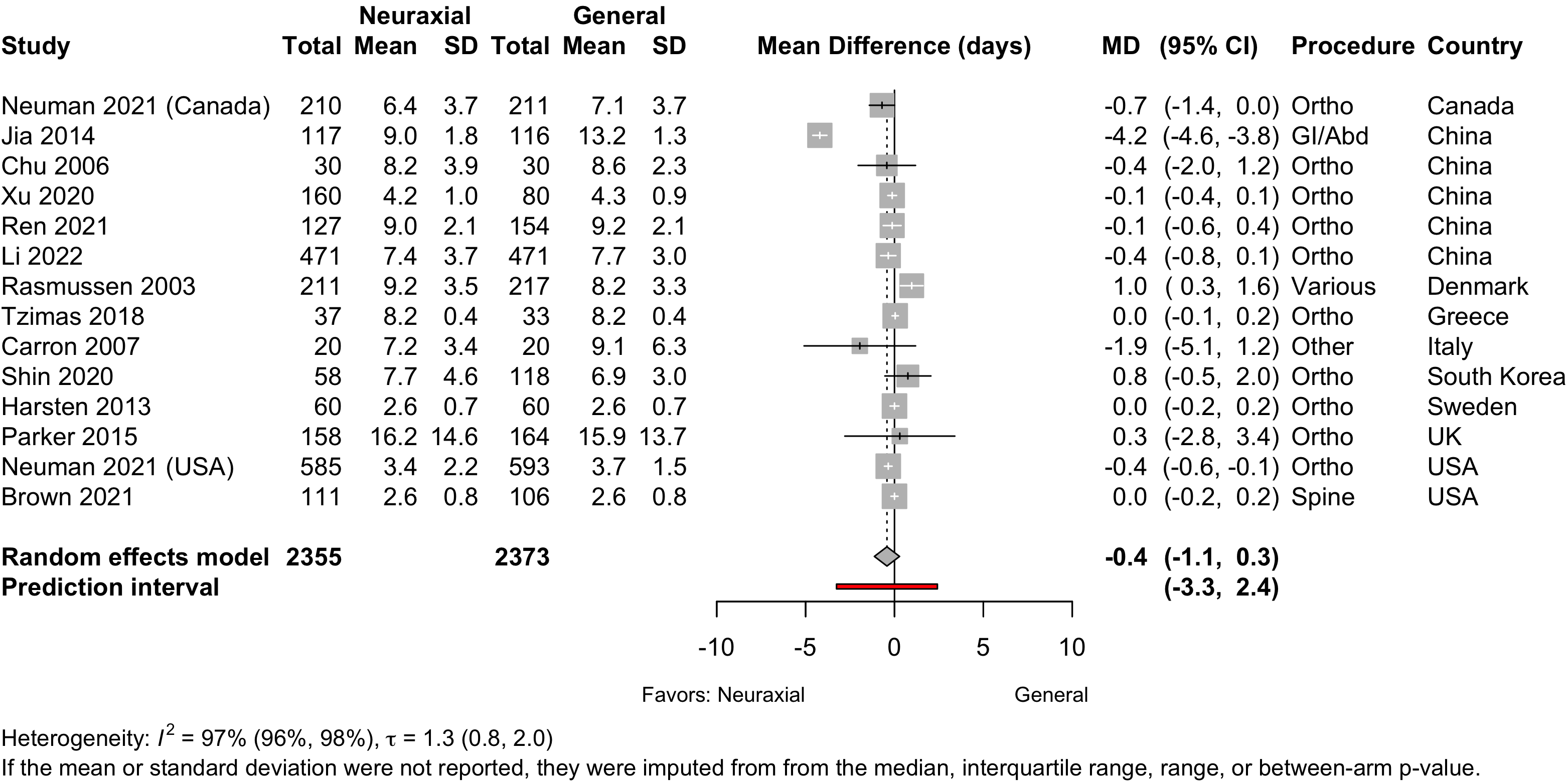
| Length of stay (days) | 13 | (2,355) | (2,373) | MD | -0.4 (-1.1 to 0.3) | |
| Discharged to institution | 1 | 576 (777) | 586 (777) | RR | 0.98 (0.93-1.04) | |
| Mortality (in-hospital and 30-day) | ||||||
| All procedures | 6 | 19 (1,789) | 32 (1,859) | RR | 0.66 (0.28–1.50) | |
| 9 | 19 (1,926) | 31 (1,942) | RD/1000 | -5.4 (-12.3 to 1.5) | ||
| Hip fracture | 4 | 19 (1,467) | 28 (1,536) | — |
RR | 0.75 (0.34–1.64) |
| 5 | 19 (1,486) | 27 (1,557) | RD/1000 | -3.6 (-16.6 to 9.5) | ||
| Other | 2 | 19 (322) | 31 (323) | — |
RR | 0.20 (0.02–1.71)‡‡ |
| 4 | 0 (440) | 4 (443) | RD/1000 | -8.8 (-21.1 to 3.6) | ||
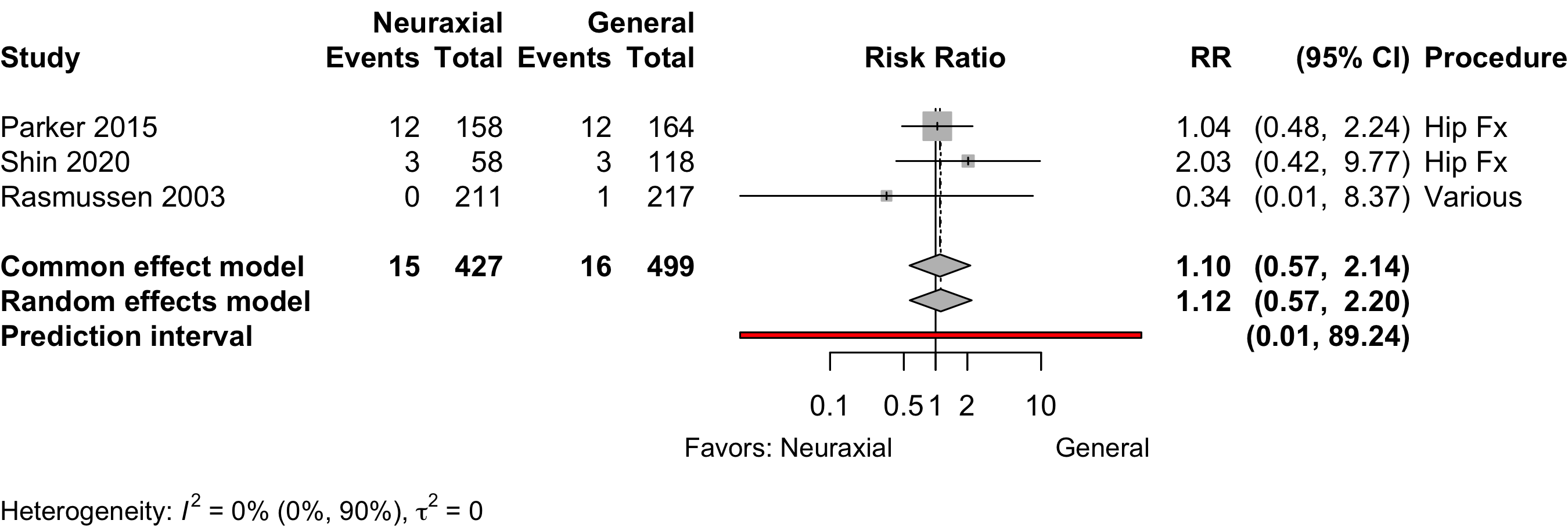
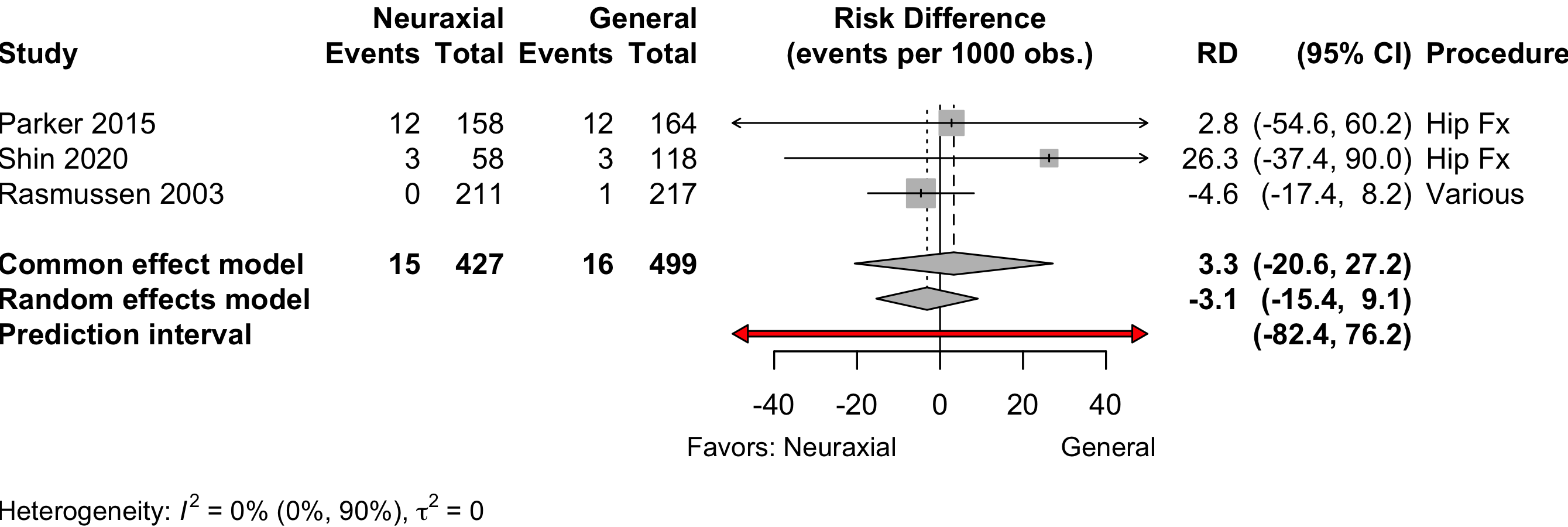
| Mortality (90-day) | 3 | 15 (427) | 16 (499) | RR | 1.12 (0.57–2.20) | |
| 3 | 15 (427) | 16 (499) | RD/1000 | -3.1 (-15.4 to 9.1) | ||
| RCT: randomized clinical trial; GRADE: Grades of Recommendation, Assessment, Development, and Evaluation; RR: risk ratio; SMD: standardized mean difference; MD: mean difference; RD/1000: risk difference per 1000. | ||||||
| * Very low: ⨁◯◯◯; Low: ⨁⨁◯◯; Moderate: ⨁⨁⨁◯; High: ⨁⨁⨁⨁. | ||||||
| † Hip fracture trials (n = 6) RR 1.08 (95% CI, 0.87–1.35); other procedures (n = 4) RR 0.74 (95% CI, 0.35–1.57). | ||||||
| ‡ RD per 100 for all surgeries 0.1 (-1.8 to 2.2); in hip fracture trials 1.3 (-1.3 to 3.9); others -2.2 (-9.2 to 4.8). | ||||||
| § Using Neuman 2021 primary result of inability to walk 60 feet without human assistance in a sensitivity analysis including 1644 patients yield a pooled SMD -0.07 (95% CI, -0.25 to 0.12). | ||||||
| ** Complications reported variously across the 13 trials. | ||||||
| †† Comparing higher/highest category or categories with lower ones. | ||||||
| ‡‡ Common effects model (2 trials). | ||||||
Neuraxial versus General Anesthesia
Key Question
Among older patients undergoing surgery and anesthesia, does neuraxial anesthesia as the primary anesthetic approach improve postoperative outcomes compared with general anesthesia?
Balance Tables
Benefits, harms, and strength of evidence (GRADE) for neuraxial versus general anesthesia.
Included complications and strength of evidence (GRADE) for neuraxial versus general anesthesia.
| Outcome | RCT | Neuraxial | General | GRADE* | Effect† | Estimate (95% CI) |
|---|---|---|---|---|---|---|
| N (Total) | N (Total) | |||||
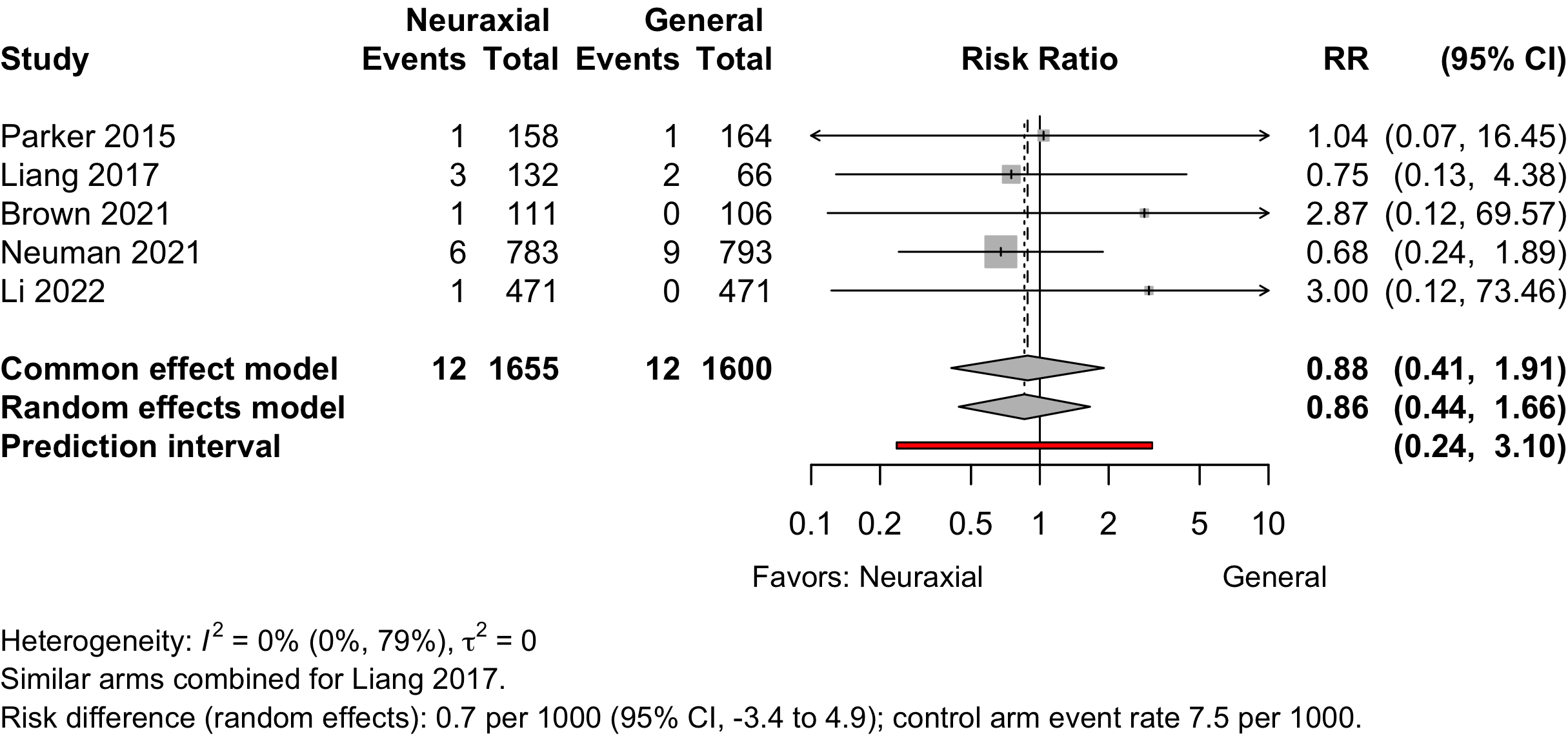
| Myocardial infarction | 5 | 12 (1,655) | 12 (1,600) | RR | 0.86 (0.44–1.66) | |
| RD/1000 | 0.7 (-3.4 to 4.9) | |||||
| Cardiac arrest | 1 | 2 (783) | 0 (793) | RD/1000 | 2.6 (-2.2 to 6.7) | |
| Bradycardia | 3 | 6 (67) | 4 (67) | RR | 1.33 (0.14–13.0) | |
| 4 | 6 (107) | 4 (107) | RD/1000 | 10.4 (-39.7 to 60.6) | ||
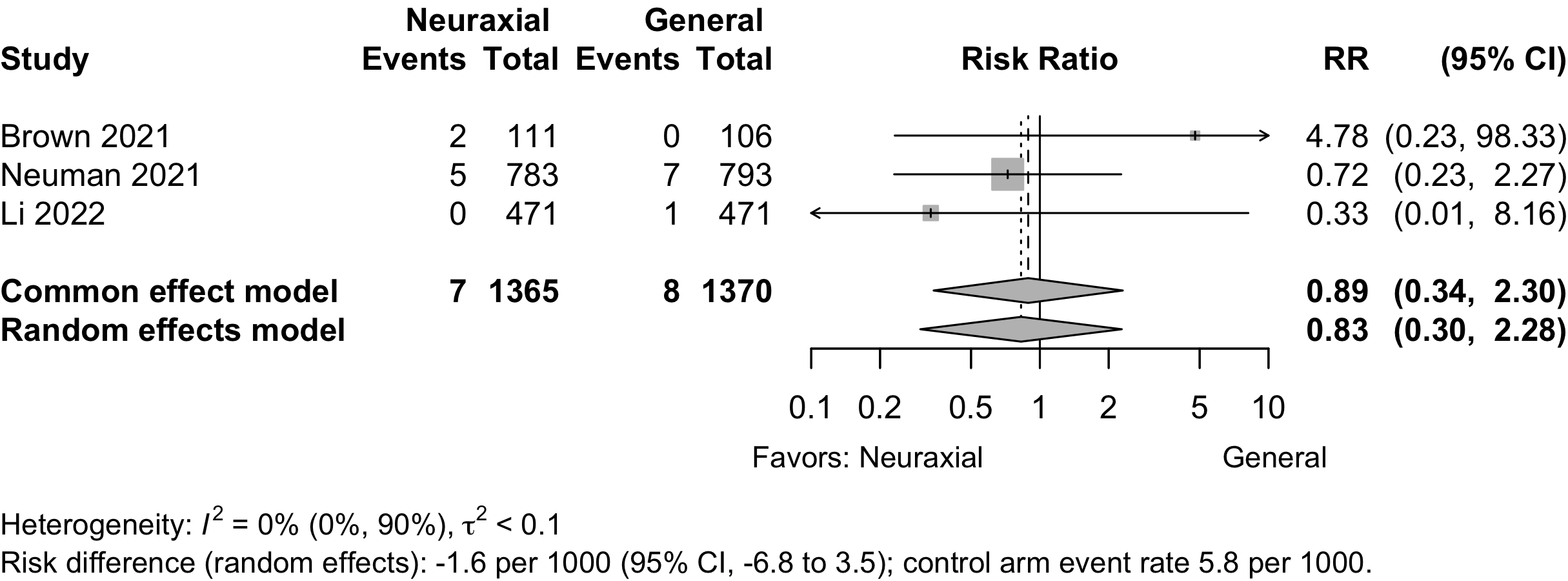
| Stroke | 3 | 7 (1,365) | 8 (1,370) | RR | 0.83 (0.30–2.28) | |
| RD/1000 | -1.6 (-6.8 to 3.5) | |||||
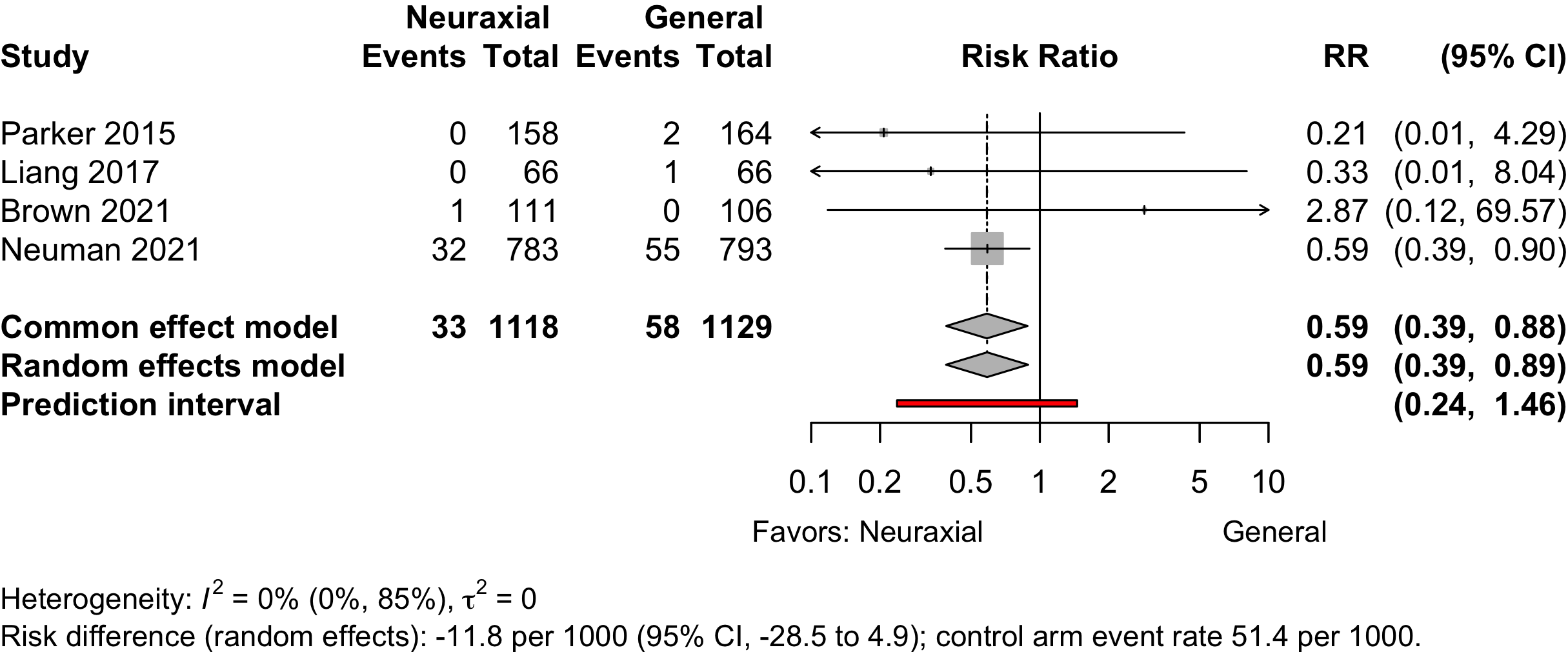
| Acute Kidney Injury | 4 | 33 (1,118) | 58 (1,129) | RR | 0.59 (0.39–0.89) | |
| RD/1000 | -21.7 (-38.1 to -5.3) | |||||
| Pulmonary complications‡ | 1 | 5 (58) | 9 (118) | RR | 0.90 (0.29–2.81) | |
| RD/1000 | -7.4 (-88.2 to 73.6) | |||||
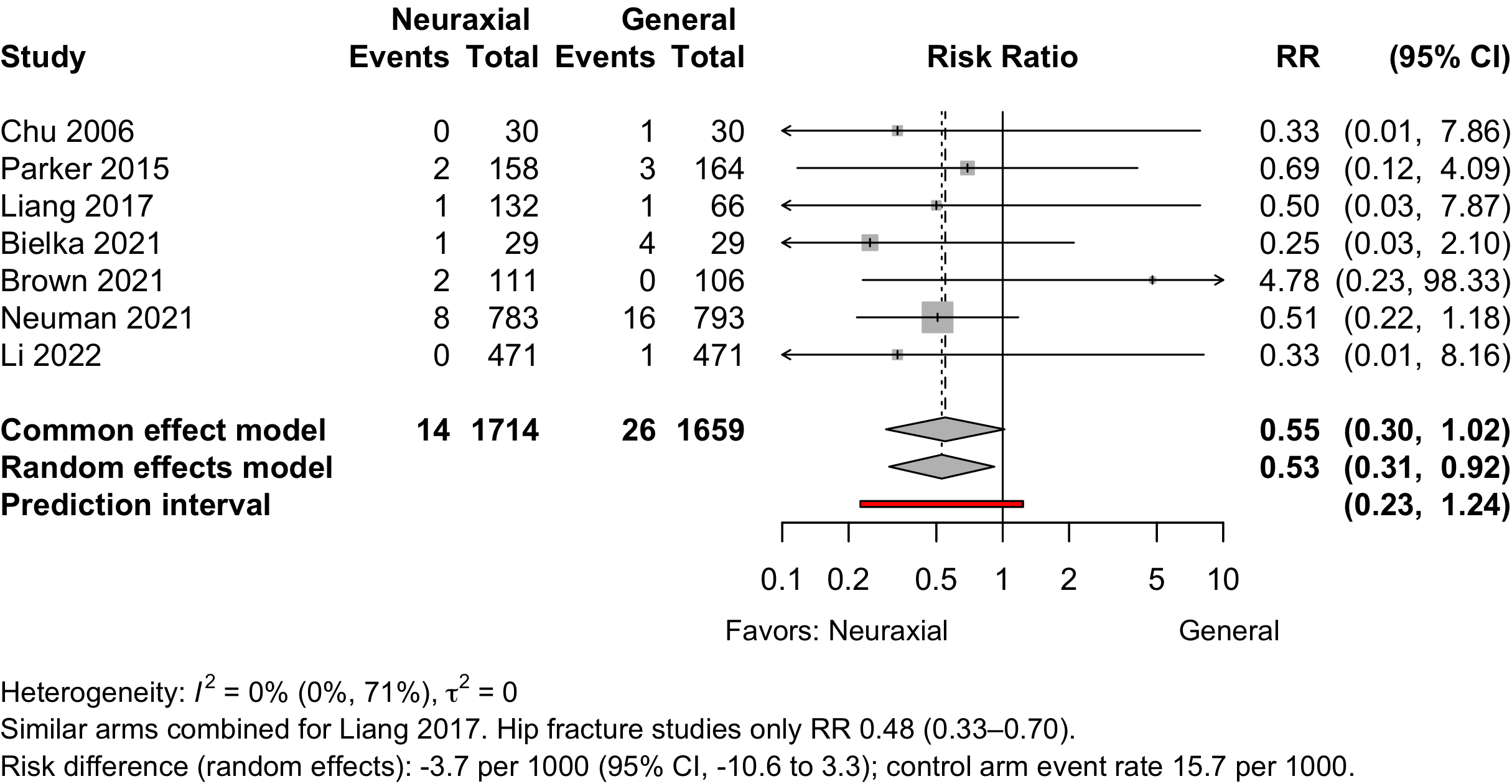
| Pneumonia | 7 | 14 (1,714) | 26 (1,659) | RR | 0.53 (0.31–0.92) | |
| RD/1000 | -7.4 (-15.0 to 0.1) | |||||
| Pulmonary congestion | 1 | 9 (783) | 8 (793) | RR | 1.14 (0.44–2.94) | |
| RD/1000 | 1.4 (-8.8 to 11.6) | |||||
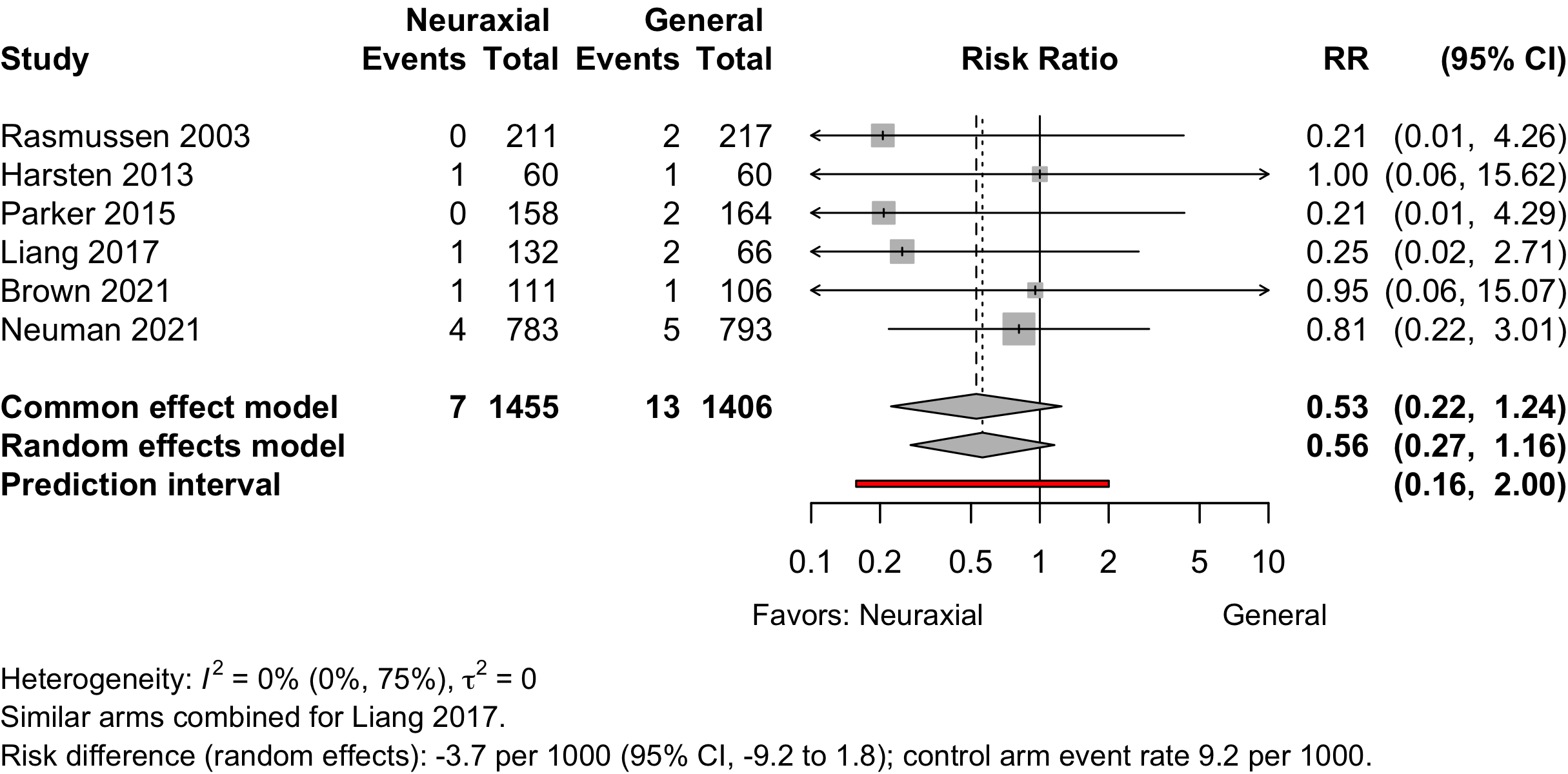
| Pulmonary embolism | 6 | 7 (1,455) | 13 (1,406) | RR | 0.56 (0.27–1.16) | |
| RD/1000 | -4.9 (-11.4 to 1.7) | |||||
| Reintubation | 1 | 4 (783) | 7 (793) | RR | 0.37 (0.17–1.97) | |
| RD/1000 | -3.7 (-11.9 to 4.5) | |||||
| RCT: randomized clinical trial; GRADE: Grades of Recommendation, Assessment, Development, and Evaluation; AKI: acute kidney injury; RR: risk ratio; RD/1000: risk difference per 1000. | ||||||
| * Very low: ⨁◯◯◯; Low: ⨁⨁◯◯; Moderate: ⨁⨁⨁◯; High: ⨁⨁⨁⨁. | ||||||
| † Fixed/common effects models when 2 studies. | ||||||
| ‡ Complications reported included pneumonia, respiratory failure, or unspecified. | ||||||
Outcomes Reported
| Outcome | RCT, N = 39a |
|---|---|
| ADL | 3 (7.7%) |
| Complications | 18 (46%) |
| DNCR/POCD | 5 (13%) |
| Delirium | 11 (28%) |
| Delirium duration | — |
| Discharge location | 2 (5.1%) |
| Mortality | 9 (23%) |
| Opioid use | 1 (2.6%) |
| Pain | 4 (10%) |
| QoR | — |
| Readmission | 2 (5.1%) |
| Satisfaction | 10 (26%) |
| ADL: activities of daily living; DNCR: delayed neurocognitive recovery; PND: postoperative neurocognitive disorder; QoR: quality of recovery; RCT: randomized clinical trial. | |
| a Number of publications, not unique trials (see inlcuded studies below). | |
| Outcome | RCT, N = 39a |
|---|---|
| Delirium duration | 1 (2.6%) |
| Length of stay | 12 (31%) |
| Opioid use | 7 (18%) |
| RCT: randomized clinical trial. | |
| a Number of publications, not unique trials (see inlcuded studies below). | |
| Outcome | RCT, N = 39a |
|---|---|
| ADL | 3 (7.7%) |
| DNCR/POCD | 10 (26%) |
| Delirium | 1 (2.6%) |
| Complications | 1 (2.6%) |
| Pain | 16 (41%) |
| Quality of life | 1 (2.6%) |
| QoR | 1 (2.6%) |
| Satisfaction | 1 (2.6%) |
| ADL: activities of daily living; DNCR: delayed neurocognitive recovery; PND: postoperative neurocognitive disorder; QoR: quality of recovery; RCT: randomized clinical trial. | |
| a Number of publications, not unique trials (see inlcuded studies below). | |
Included Studies
See Appendix for detailed summary study and patient characteristics including primary outcomes.
| Design | Studies |
|---|---|
| Randomized Clinical Trial | 37 |
| Total | 37 |
| One trial with three publications counted once. | |
Design, centers, country, and surgery
| ID | Study | Centers | Enrolled | Country | Surgery |
|---|---|---|---|---|---|
| 4782 | 1 | 198 | Chinaa | Hip fracture | |
| 13141 | 1 | 281 | Chinaa | Hip fracture | |
| 7490 | 9 | 950 | China | Hip fracture | |
| 6072 | 1 | 40 | France | Hip fracture | |
| 1320 | 1 | 72 | Greece | Hip fracture | |
| 13669 | 1 | 100 | Irana | Hip fracture | |
| 14441 | 1 | 30 | Italy | Hip fracture | |
| 6109 | 1 | 186 | South Korea | Hip fracture | |
| 1335 | 1 | 322 | UK | Hip fracture | |
| 8117 | 46 | 1600 | USA | Hip fracture | |
| 17100 | 46 | 1600 | USA | Hip fracture | |
| 18678 | 46 | 1600 | USA | Hip fracture | |
| 6540 | 1 | 90 | Ukrainea | Hip fracture | |
| 14566 | 1 | 60 | Chinaa | Ortho | |
| 1489 | 1 | 80 | Chinaa | Ortho | |
| 2020 | 1 | 25 | Chinaa | Ortho | |
| 158 | 1 | 240 | Chinaa | Ortho | |
| 5894 | 1 | 60 | Indiaa | Ortho | |
| 17971 | 1 | 210 | Malta | Ortho | |
| 208 | 1 | 124 | Sweden | Ortho | |
| 269 | 1 | 120 | Sweden | Ortho | |
| 2252 | 1 | 80 | Turkey | Ortho | |
| 781 | 1 | 98 | Australia | Urol | |
| 296 | 1 | 72 | Italy | Urol | |
| 329 | 1 | 121 | Italy | Urol | |
| 397 | 1 | 80 | Japan | Urol | |
| 737 | 1 | 60 | Turkeya | Urol | |
| 3218 | 1 | 61 | USA | Urol | |
| 16573 | 1 | 240 | Chinaa | GI/Abdominal | |
| 6132 | 1 | 206 | Chinaa | GI/Abdominal | |
| 658 | 1 | 54 | Thailand | GI/Abdominal | |
| 241 | 1 | 57 | Croatia | Neuro | |
| 15278 | 1 | 52 | Turkey | Neuro | |
| 262 | 1 | 60 | UK | Gyn | |
| 1400 | 1 | 50 | Greece | Gyn|Ortho|Urol|Vasc | |
| 7554 | 1 | 219 | USA | Spine | |
| 307 | 1 | 40 | Croatia | Vasc | |
| 831 | 12 | 428 | Denmark | Variousb | |
| 239 | 1 | 40 | Italy | Otherc | |
| GI: gastrointestinal; Ortho: orthopedic; Urol: urological; Neuro: neurological; Vasc: vascular; Various: described as various/mixed or more than 4 different tyeps of procedures. | |||||
| a Non very-high Human Development Index country. | |||||
| b Described as various or more than 4 different types of surgery. | |||||
| c Loco-regional antiblastic perfusion with circulatory block. | |||||
Country Summary
| N = 37a | |
|---|---|
| Country | |
| China | 9 (24%) |
| Italy | 4 (11%) |
| Turkey | 3 (8.1%) |
| USA | 3 (8.1%) |
| Croatia | 2 (5.4%) |
| Greece | 2 (5.4%) |
| Sweden | 2 (5.4%) |
| UK | 2 (5.4%) |
| Australia | 1 (2.7%) |
| Denmark | 1 (2.7%) |
| France | 1 (2.7%) |
| India | 1 (2.7%) |
| Iran | 1 (2.7%) |
| Japan | 1 (2.7%) |
| Malta | 1 (2.7%) |
| South Korea | 1 (2.7%) |
| Thailand | 1 (2.7%) |
| Ukraine | 1 (2.7%) |
| a n (%) | |
Comparators
| Study | N | Arm | ASA | Agea | MMSEa | Dementia N (%)b |
General | Neuraxial | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PS | Vol | TIVA | NR | Spinal | Epid | CSE | ||||||
| Ortho — HipFx | ||||||||||||
| 15 | Gen | 23 | 84.0 [67-88] |
29 [24-29] |
● | |||||||
| 15 | Neur | 84.0 [71-94] |
28 [25-30] |
● | ||||||||
| 164 | Gen | 1234 | 83.0 [59-99] |
● | ||||||||
| 158 | Neur | 82.9 [25-105] |
● | |||||||||
| 50 | Gen | 123 | 66.0 (4.8) |
0 (0) | ● | |||||||
| 50 | Neur | 66.2 (5.2) |
0 (0) | ● | ||||||||
| 66 | Gen | 123 | 68.0 (11.0) |
26.7 (1.6) |
0 (0) | ● | ||||||
| 66 | Neur | 67.0 (12.0) |
26.8 (2.0) |
0 (0) | ● | |||||||
| 66 | Neur | 66.0 (10.0) |
26.6 (1.9) |
0 (0) | ● | |||||||
| 21 | Gen | 123 | 85.0 (5.0) |
21 [12-24] |
● | |||||||
| 19 | Neur | 83.0 (6.0) |
19 [12-26] |
● | ||||||||
| 33 | Gen | 123 | 75.1 (6.1) |
25.7 (2.9) |
0 (0) | ● | ||||||
| 37 | Neur | 77.1 (6.5) |
25.3 (0.9) |
0 (0) | ● | |||||||
| 60 | Gen | NR | 79.4 (7.7) |
12 (20.0) | ● | |||||||
| 58 | Gen | 80.5 (6.7) |
7 (12.1) | ● | ||||||||
| 58 | Neur | 81.6 (6.7) |
10 (17.2) | ● | ||||||||
| 30 | Gen | NR | 73.0 {72-74} |
0 (0) | ● | |||||||
| 30 | Neur | 72.0 {70-73} |
0 (0) | ● | ||||||||
| 804 | Gen | 1234 | 78.4 (10.6) |
94 (11.7) | ● | |||||||
| 795 | Neur | 77.7 (10.7) |
109 (13.7) | ● | ||||||||
| 154 | Gen | 123 | 74.1 (4.2) |
25.6 (1.4) |
0 (0) | ● | ||||||
| 127 | Neur | 73.1 (6.2) |
25.7 (1.2) |
0 (0) | ● | |||||||
| 471 | Gen | 1234 | 77.0 {71-82} |
20 {15-25} |
190 (40.3) | ● | ● | |||||
| 471 | Neur | 77.0 {72-82} |
20 {15-24} |
182 (38.6) | ● | ● | ● | |||||
| 796 | Gen | 1234 | 78.0 (11.0) |
93 (11.7) | ● | |||||||
| 785 | Neur | 78.0 (11.0) |
109 (13.9) | ● | ||||||||
| 211 | Gen | NR | 211 (100) | ● | ● | |||||||
| 225 | Neur | 225 (100) | ● | |||||||||
| 418 | Gen | NR | 0 (0) | ● | ● | |||||||
| 408 | Neur | 0 (0) | ● | |||||||||
| Ortho — HipFx|Other | ||||||||||||
| 40 | Gen | NR | 69.4 (2.6) |
0 (0) | ● | |||||||
| 40 | Neur | 69.4 (2.6) |
0 (0) | ● | ||||||||
| Ortho — TKA|THA|HipFx|Other | ||||||||||||
| 30 | Gen | 12 | 67.1 (7.1) |
27.3 (1.8) |
0 (0) | ● | ||||||
| 30 | Neur | 66.6 (5.6) |
28.0 (1.3) |
0 (0) | ● | |||||||
| Ortho — TKA | ||||||||||||
| 30 | Gen | 123 | 69.0 {62-74} |
● | ||||||||
| 30 | Neur | 65.0 {62-68} |
● | |||||||||
| 60 | Gen | 123 | 68.0 (7.0) |
● | ||||||||
| 60 | Neur | 67.0 (7.0) |
● | |||||||||
| 26 | Gen | NR | 68.8 (4.9) |
22.6 (3.0) |
0 (0) | ● | ||||||
| 31 | Neur | 69.8 (4.4) |
22.6 (2.7) |
0 (0) | ● | |||||||
| 101 | Gen | 12 | 68.0 {61-71} |
● | ● | |||||||
| 99 | Neur | 68.0 {62-70} |
● | |||||||||
| Ortho — THA | ||||||||||||
| 60 | Gen | 123 | 68.0 (9.0) |
● | ||||||||
| 58 | Neur | 66.0 (7.8) |
● | |||||||||
| 80 | Gen | NR | 75.4 (5.6) |
● | ||||||||
| 80 | Neur | 75.6 (5.5) |
● | |||||||||
| 80 | Neur | 75.0 (5.2) |
● | |||||||||
| Ortho | ||||||||||||
| 13 | Gen | NR | 58.4 (7.3) |
● | ||||||||
| 12 | Neur | 62.7 (8.7) |
● | |||||||||
| Urol | ||||||||||||
| 34 | Gen | NR | 66.0 (6.8) |
● | ||||||||
| 36 | Neur | 65.3 (6.9) |
● | |||||||||
| 34 | Gen | NR | 66.0 (7.0) |
● | ||||||||
| 30 | Neurd | 59.5 (10.4) |
● | |||||||||
| 29 | Neure | 64.1 (8.1) |
● | |||||||||
| 28 | Neurf | 65.3 (6.3) |
● | |||||||||
| 40 | Gen | 12 | 73.0 (6.0) |
0 (0) | ● | |||||||
| 40 | Neur | 71.0 (6.0) |
0 (0) | ● | ||||||||
| 30 | Gen | 23 | 70.0 (9.6) |
● | ||||||||
| 30 | Neur | 76.4 (11.8) |
● | |||||||||
| 50 | Gen | NR | 63.9 [55-78] |
0 (0) | ● | |||||||
| 48 | Neur | 66.9 [56-75] |
0 (0) | ● | ||||||||
| 29 | Gen | NR | 63.7 (11.4) |
● | ||||||||
| 29 | Neur | 67.3 (10.9) |
● | |||||||||
| GI/Abdominal | ||||||||||||
| 116 | Gen | NR | 74.8 (4.0) |
0 (0) | ● | |||||||
| 117 | Neur | 75.7 (4.2) |
0 (0) | ● | ||||||||
| 103 | Gen | NR | 71.9 (8.4) |
● | ||||||||
| 103 | Neur | 71.2 (7.9) |
● | |||||||||
| 18 | Gen | 123 | 67.7 (15.1) |
● | ||||||||
| 18 | Neur | 64.9 (10.3) |
● | |||||||||
| Neuro | ||||||||||||
| 28 | Gen | NR | 66.0 (8.7) |
● | ||||||||
| 29 | Neur | 66.2 (8.3) |
● | |||||||||
| 25 | Gen | 123 | 62.7 (14.3) |
0 (0) | ● | |||||||
| 25 | Neur | 67.0 (10.4) |
0 (0) | ● | ||||||||
| Gyn | ||||||||||||
| 28 | Gen | 123 | 65.1 (12.5) |
● | ||||||||
| 31 | Neur | 60.6 (11.5) |
● | |||||||||
| Gyn|Ortho|Urol|Vasc | ||||||||||||
| 28 | Gen | 1234 | ≥60 |
28.1 |
0 (0) | ● | ● | |||||
| 19 | Neur | ≥60 |
27.6 |
0 (0) | ● | ● | ||||||
| Spine | ||||||||||||
| 106 | Gen | NR | 72.0 {69-76} |
28 {27-29} |
0 (0) | ● | ||||||
| 111 | Neur | 73.0 {69-78} |
29 {27-29} |
0 (0) | ● | |||||||
| Vasc | ||||||||||||
| 20 | Gen | 23 | 61.2 (10.5) |
● | ||||||||
| 20 | Neur | 60.6 (9.7) |
● | |||||||||
| Various | ||||||||||||
| 217 | Gen | 1234 | 70.8 [61-84] |
0 (0) | ● | |||||||
| 211 | Neur | 71.1 [61-84] |
0 (0) | ● | ● | |||||||
| Other | ||||||||||||
| 20 | Gen | 123 | 62.6 (10.7) |
● | ||||||||
| 20 | Neur | 65.5 (16.8) |
● | |||||||||
| Gen: general; Neur: neuraxial; PS: physical stutus; Vol: volatile; TIVA: total intravenous anesthesia; NR: not reported; Epid: epidural; CSE: combined spinal and epidural; Ortho: orthopedic; Urol: urological; GI: gastrointestinal; Neuro: neurologic; Gyn: gynecologic; Vasc: vascular; Ophtho: opthalomogic; Fx: fracture; TKA: total knee arthroplasty; THA: total hip arthroplasty. | ||||||||||||
| a Mean Med (SD)[Range]{IQR}. | ||||||||||||
| b Blank if no information provided. | ||||||||||||
| c Analysis of Neuman 2021. | ||||||||||||
| d Propofol. | ||||||||||||
| e Midazolam. | ||||||||||||
| f Diazepam. | ||||||||||||
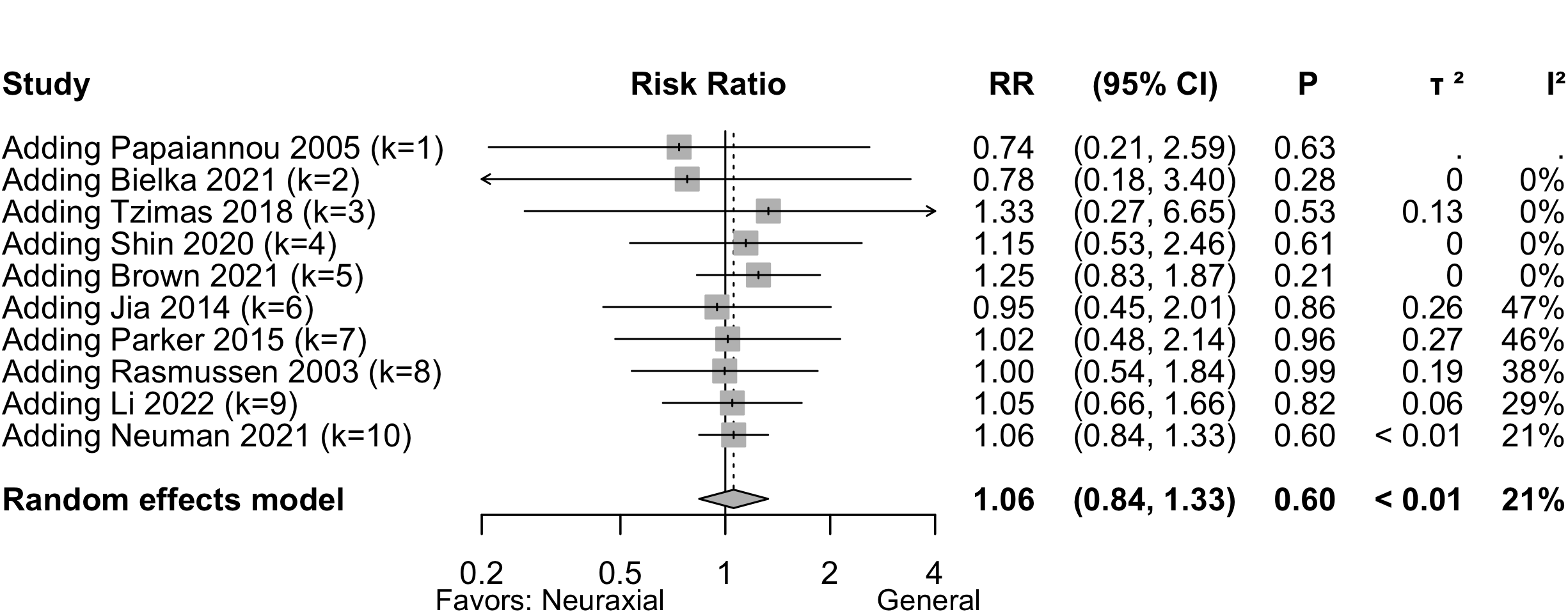
Delirium Incidence
| Study | N | Arm | MMSE (preop)a |
Dementia N (%)b |
Scale | Day(s)c | Incidence Proportion | RR (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|
| N (%) | 0 – 100% | ||||||||
| Hip Fx | |||||||||
| 164 | Gen | unspecified | Stay | 0 (0) | — | ||||
| 158 | Neur | 3 (1.9) | Not estimated | ||||||
| 33 | Gen | 25.7 (2.9) |
0 (0) | CAM | Stay | 4 (12.1) | — | ||
| 37 | Neur | 25.3 (0.9) |
0 (0) | 10 (27.0) | 2.23 (0.77-6.44) | ||||
| 118 | Gen | 22 (18.6) | unspecified | Stay | 17 (14.4) | — | |||
| 58 | Neur | 10 (17.2) | 8 (13.8) | 0.96 (0.44-2.09) | |||||
| 30 | Gen | 0 (0) | DSM | Stay | 1 (3.3) | — | |||
| 30 | Neur | 0 (0) | 1 (3.3) | 1.00 (0.07-15.26) | |||||
| 629 | Gen | 94 (11.7) | CAM | 3 | 124 (19.7) | — | |||
| 633 | Neur | 109 (13.7) | 130 (20.5) | 1.04 (0.84-1.30)e | |||||
| 467 | Gen | 20 {15-25} |
190 (40.3) | CAM | 7 | 21 (4.5) | — | ||
| 466 | Neur | 20 {15-24} |
182 (38.6) | 24 (5.2) | 1.15 (0.65-2.03) | ||||
| 190 | Gen | 18 (100) | CAM | 7 | 18 (9.5) | — | |||
| 182 | Neur | 21 (100) | 21 (11.5) | 1.22 (0.67-2.21) | |||||
| 281 | Gen | 0 (0) | CAM | 7 | 6 (2.1) | — | |||
| 289 | Neur | 0 (0) | 8 (2.8) | 1.30 (0.46-3.69) | |||||
| 211 | Gen | 64 (100) | CAM | Stay | 64 (30.3) | — | |||
| 225 | Neur | 71 (100) | 71 (31.6) | 1.04 (0.79-1.38)f | |||||
| 418 | Gen | 0 (0) | CAM | Stay | 60 (14.4) | — | |||
| 408 | Neur | 0 (0) | 59 (14.5) | 1.01 (0.72-1.40)g | |||||
| GI/Abd | |||||||||
| 116 | Gen | 0 (0) | DRS | Stay | 15 (12.9) | — | |||
| 117 | Neur | 0 (0) | 4 (3.4) | 0.26 (0.09-0.77) | |||||
| Spine | |||||||||
| 106 | Gen | 28 {27-29} |
0 (0) | CAM | Stay | 20 (18.9) | — | ||
| 111 | Neur | 29 {27-29} |
0 (0) | 28 (25.2) | 1.34 (0.80-2.22) | ||||
| Various | |||||||||
| 217 | Gen | 0 (0) | unspecified | Stay | 5 (2.3) | — | |||
| 211 | Neur | 0 (0) | 4 (1.9) | 0.82 (0.22-3.02) | |||||
| 28 | Gen | 28.1 |
0 (0) | DSM | 3 | 6 (21.4) | — | ||
| 19 | Neur | 27.6 |
0 (0) | 3 (15.8) | 0.74 (0.21-2.59) | ||||
| Gen: general anesthesia; Neur: neuraxial; RR: risk ratio; MMSE: Mini-Mental State Examination; CAM: Confusion Assessment Method; DRS: Delirium Rating Scale; DSM: Diagnostic and Statistical Manual of Mental Disorders; NR: not reported. | |||||||||
| a Mean Med (SD)[Range]{IQR}. | |||||||||
| b Blank if no information provided. | |||||||||
| c Day(s) over which incidence proportion assessed. Stay indicates duration of hospitalization. | |||||||||
| d Included patients with dementia (O'Brien 2023 report of Neuman 2021; 16.5% of patients in Shin 2020 had dementia, but subgroup results were unreported). | |||||||||
| e Adjusted for sex, fracture type and country. | |||||||||
| f Odds ratio adjusted for sex, fracture type and country 1.08 (95% CI, 0.72–1.62). | |||||||||
| g Odds ratio adjusted for sex, fracture type and country 1.01 (95% CI, 0.69–1.50). | |||||||||
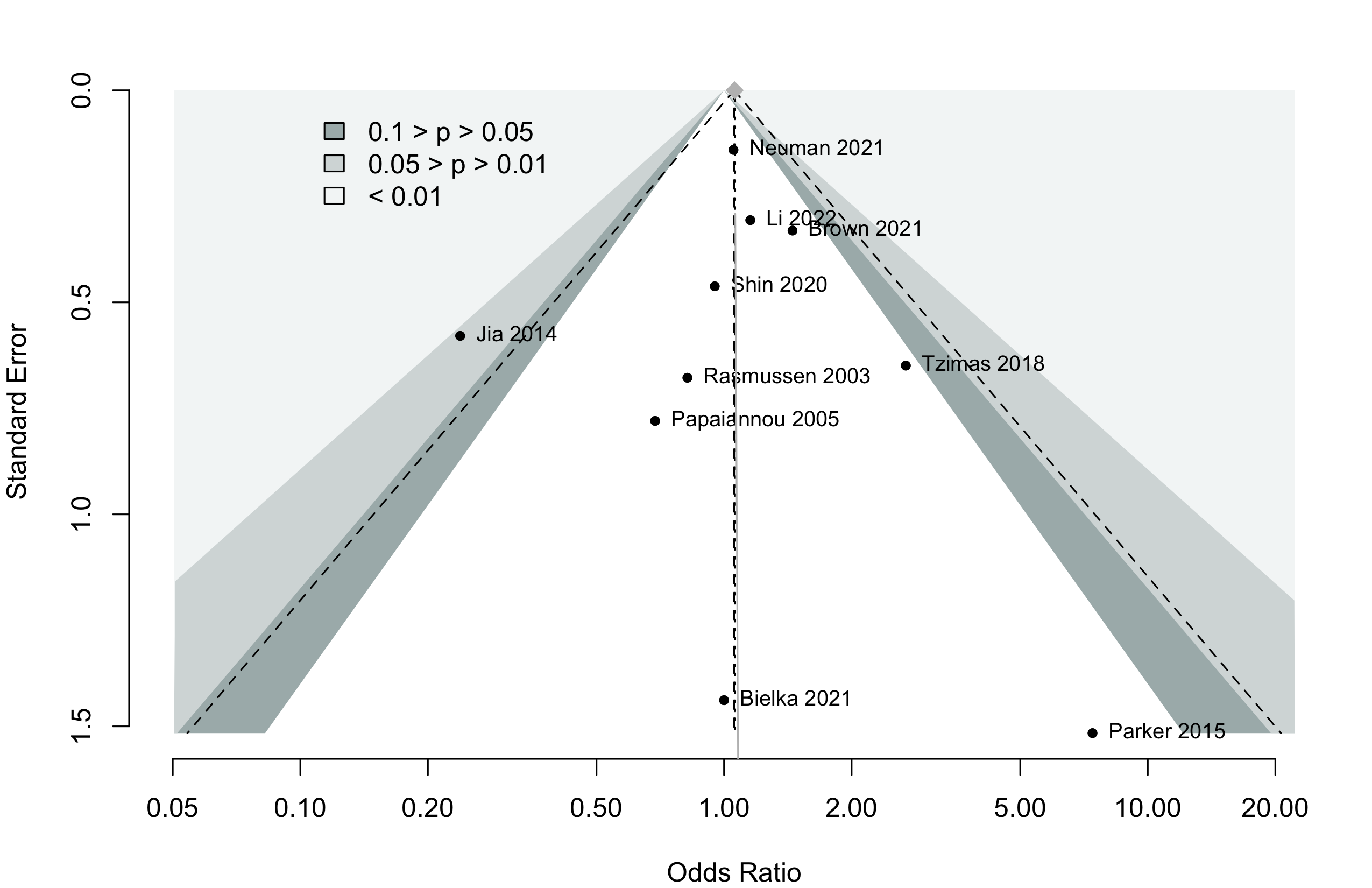
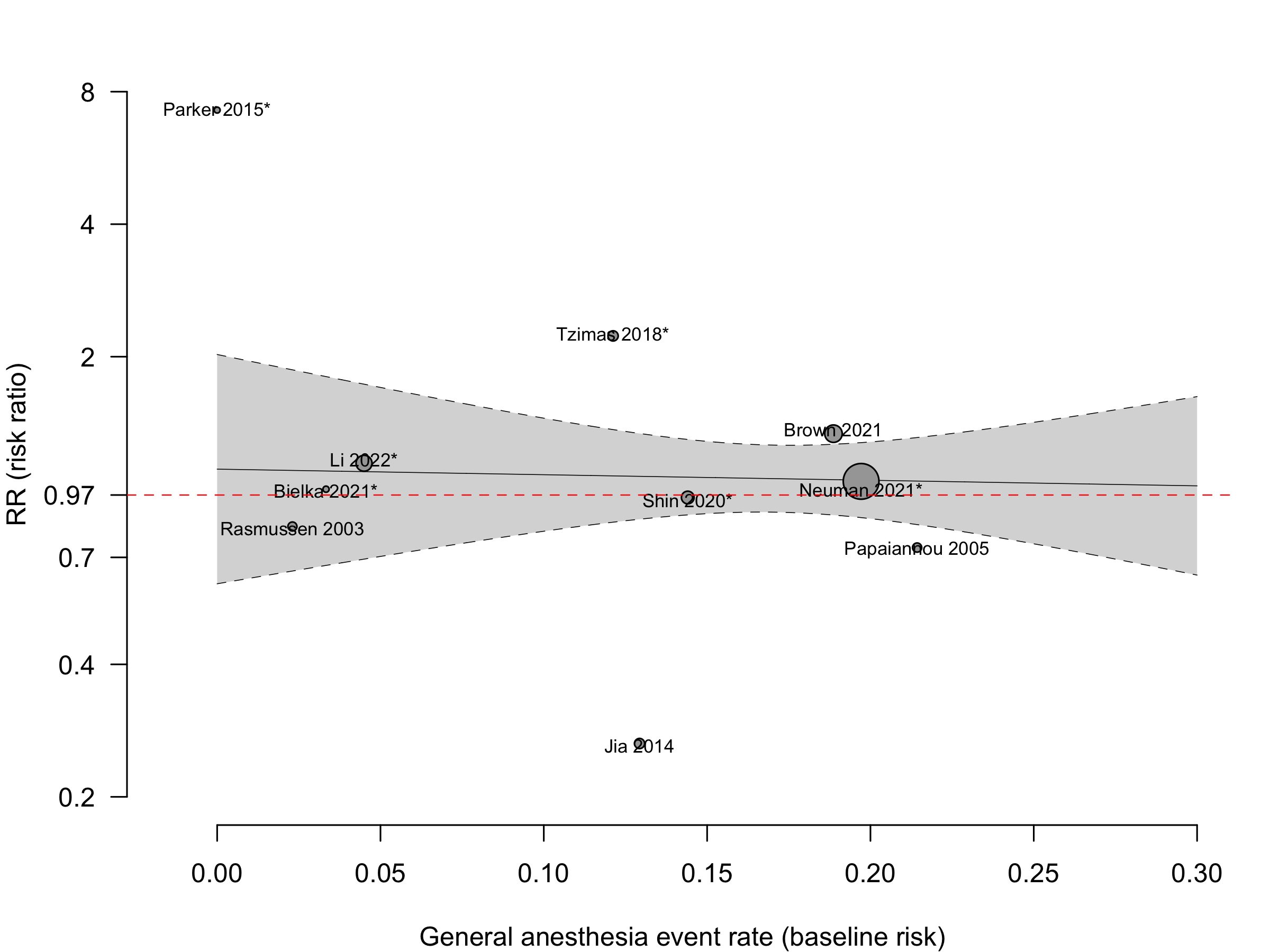
Pooled
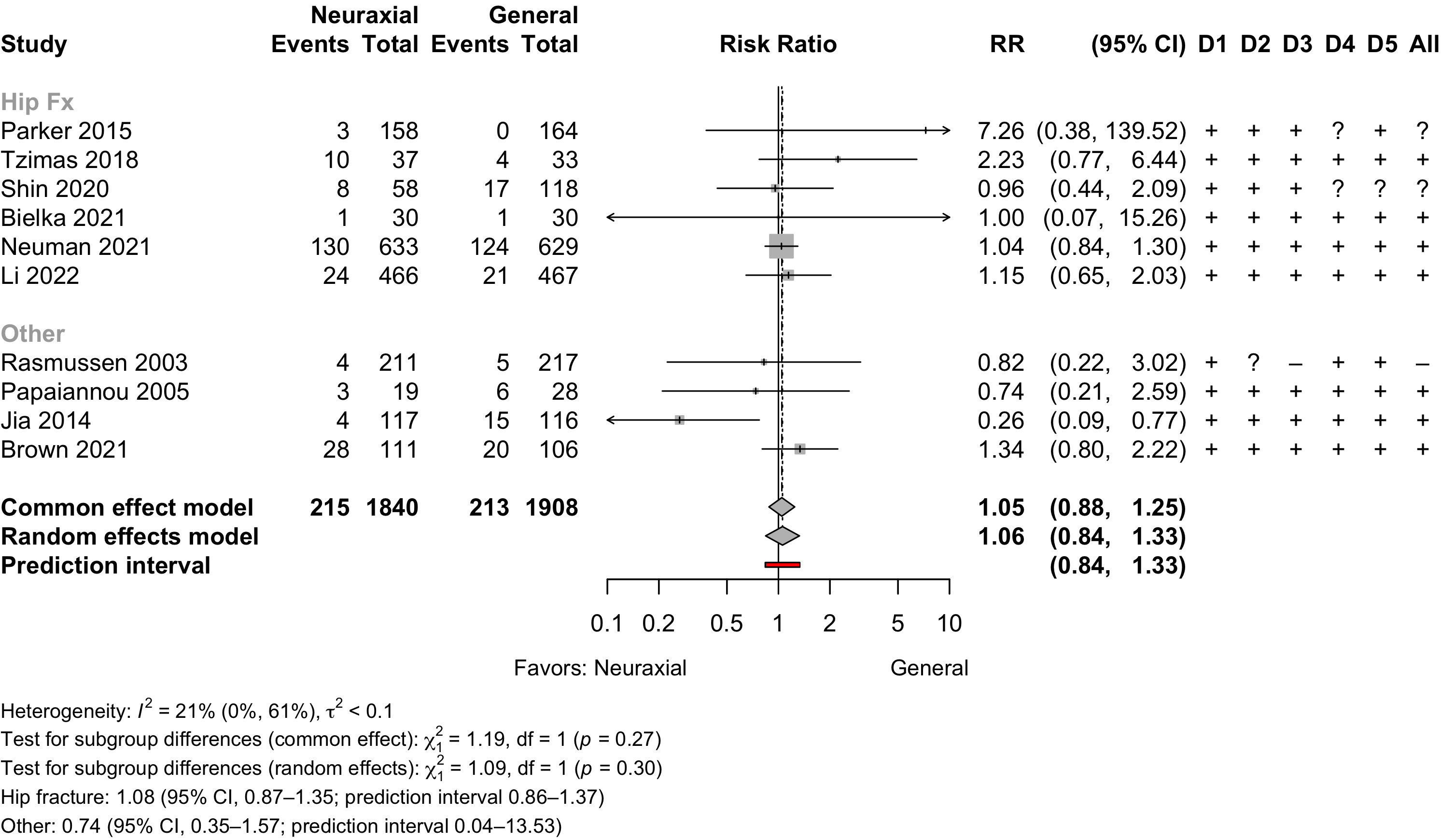
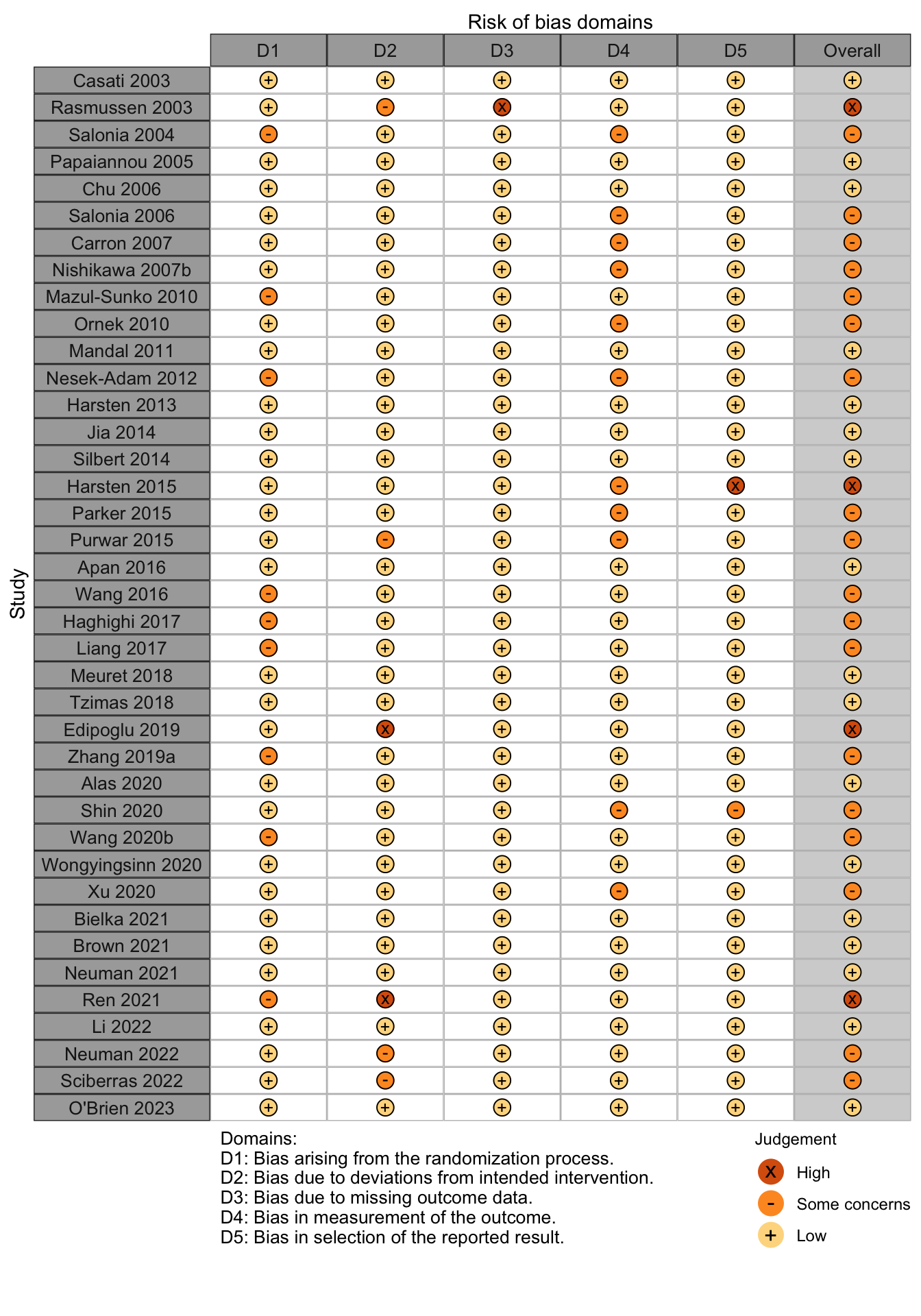
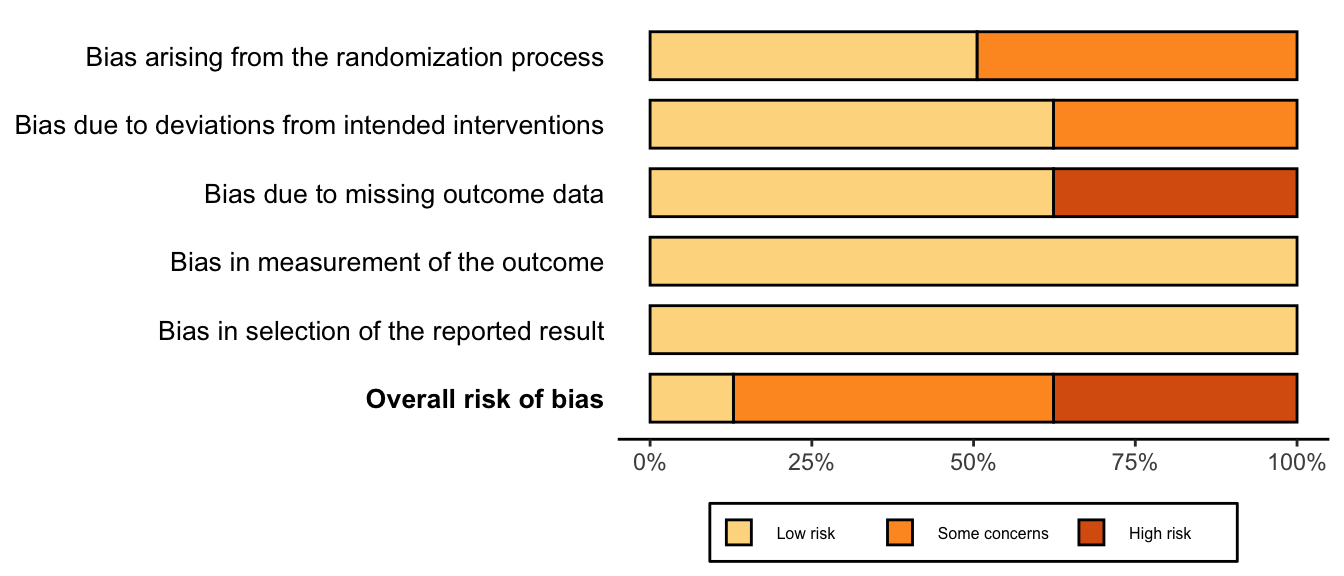
Risk of bias ratings: low +, some concerns ?, high – .
Random effects pooled estimate weights — Neuman 2021 (63.6%), Brown 2021 (11.9%), Li 2022 (9.4%), and Shin 2020 (5.1%).
Harbord test for small study effects P = 0.87.
Delirium was designated a primary or secondary outcome in 45.5% and 18.2% of trials, respectively.
In subgroups from O’Brien 2023 (Neuman 2021) and Li 2022 of patients with dementia RR 1.08 (95% CI, 0.83–1.39; common effects model).
In 8 studies including or reporting results for patients without dementia RR 1.03 (95% CI, 0.67–1.57; prediction interval 0.54–1.97).
Neurocognitive Disorder
<30 days
| Study | N | Arm | Dementiaa | Preop | Instrument | Dayc | Neurocognitive Disorder <30 days | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MMSEb | MMSE | DST | MoCA | Other | N (%) | 0 — 100% | RR (95% CI) | |||||
| 15 | Gen | 29 [24-29] |
✓d |
7 | 3 (20.0) | — | ||||||
| 15 | Neur | 28 [25-30] |
1 (6.7) | 0.33 (0.04-2.85) | ||||||||
| 188 | Gen | 0 (0) | e | 7 | 37 (19.7) | — | ||||||
| 176 | Neur | 0 (0) | 22 (12.5) | 0.64 (0.39-1.03) | ||||||||
| 49 | Gen | 0 (0) | e | 7 | 2 (4.1) | — | ||||||
| 42 | Neur | 0 (0) | 5 (11.9) | 2.92 (0.60-14.26) | ||||||||
| 103 | Gen | f | g | 7 | 46 (44.7) | — | ||||||
| 103 | Neur | f | 50 (48.5) | 1.09 (0.81-1.46) | ||||||||
| Mini-Mental State Exam; DST: Digit Span Test; MoCA: Montreal Cognitive Assessment; RR: risk ratio; Gen: general anesthesia. | ||||||||||||
| a Blank if no information provided. | ||||||||||||
| b Mean Med (SD)[Range]{IQR}. | ||||||||||||
| c Day of assessment (excluded Zhang 2019a conducting assessment at day 1). | ||||||||||||
| d Difference from baseline >2 points. | ||||||||||||
| e Z ≥1.96. | ||||||||||||
| f Did not state excluding patients with dementia, but peformed neuropsycholgical testing prior to surgery | ||||||||||||
| g Not reported. | ||||||||||||
Pooled
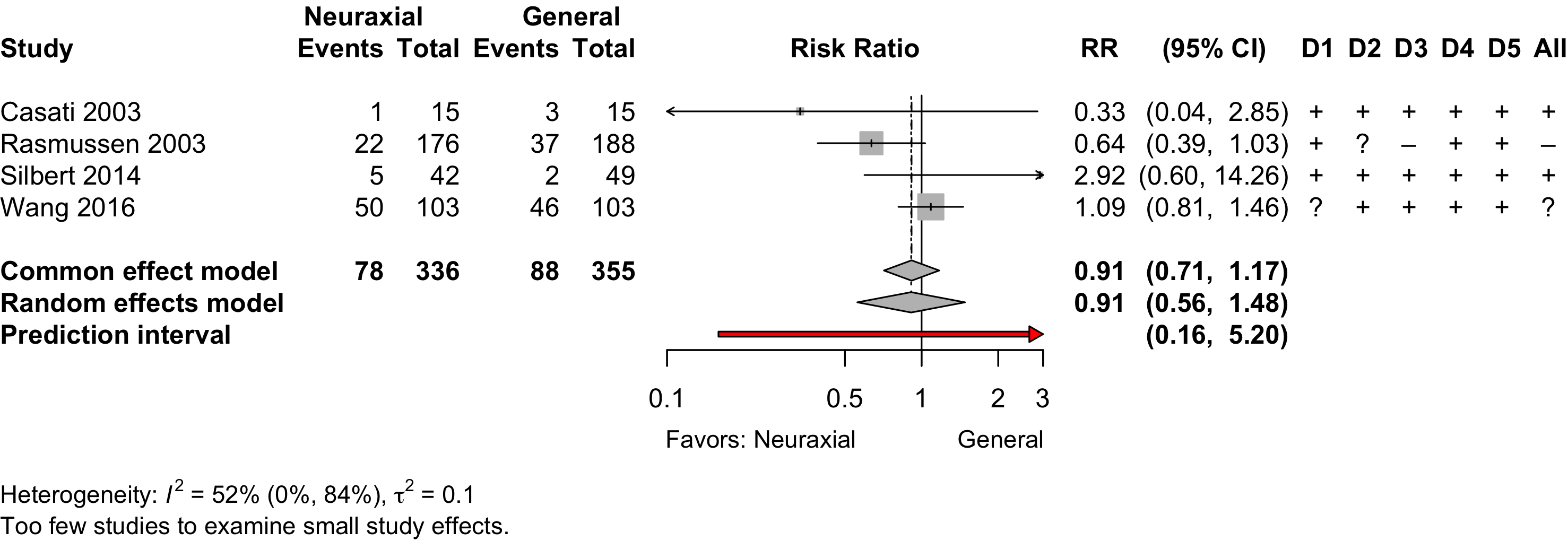
- Inverse variance method (random effects model)
- Restricted maximum-likelihood estimator for τ2
- Q-Profile method for confidence interval of τ2 and τ
- Prediction interval based on t-distribution (df = 2)
Neurocognitive Disorder
30 days to 1 year
| Study | N | Arm | Dementia | Preop | Instrument | Dayb | Postoperative Neurocognitive Disorder | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MMSEa | MMSE | DST | MoCA | Other | N (%) | 0 — 100% | RR (95% CI) | |||||
| Randomized Clinical Trial | ||||||||||||
| 188 | Gen | 0 (0) | c | 90 | 25 (13.3) | — | ||||||
| 176 | Neur | 0 (0) | 23 (13.1) | 0.98 (0.58-1.67) | ||||||||
| Mini-Mental State Exam; DST: Digit Span Test; MoCA: Montreal Cognitive Assessment; RR: risk ratio; Gen: general anesthesia. | ||||||||||||
| a Mean Med (SD)[Range]{IQR}. | ||||||||||||
| b Day of assessment. | ||||||||||||
| c Z ≥1.96. | ||||||||||||
Physical Function
| Study | N | Arma | Unable to Walk N (%)b |
0 — 100% | RR (95% CI) |
|---|---|---|---|---|---|
| 701 | Gen | 101 (14.4) | |||
| 684 | Neur | 104 (15.2) | 1.05 (0.82–1.36)c | ||
| a Gen: general anesthesia; Neur: neuraxial anesthesia. | |||||
| b Inability to walk without human assistance at 60 days. | |||||
| c Equivalent standardized mean difference: 0.04 (95% CI, -0.13 to 0.20). | |||||
| Study | N | Arm | Agea | Scaleb | Range | Days | Ratinga | SMD (95% CI) |
|---|---|---|---|---|---|---|---|---|
| 30-90 days | ||||||||
| 28 | Gen | 65.1 (12.5) |
SF-36 physical | 0→100 | 84 | 44.2 (8.3) |
||
| 31 | Neur | 60.6 (11.5) |
47.1 (12.7) |
0.26 (-0.25 to 0.78) | ||||
| 242 | Gen | 78.4 (10.6) |
WHODAS 2.0 | 0←100 | 60 | 18 [6-32] |
||
| 225 | Neur | 77.7 (10.7) |
23 [8-43] |
0.36 (0.18 to 0.55) | ||||
| 101 | Gen | 68.0 {61-71} |
WOMACc | 0←96 | 90 | 17.5 (14.6)d |
||
| 99 | Neur | 68.0 {62-70} |
15.0 (13.9)d |
-0.18 (-0.45 to 0.10) | ||||
| >90 days | ||||||||
| 101 | Gen | 68.0 {61-71} |
WOMACc | 0←96 | 180 | 13.8 (15.3)d |
||
| 99 | Neur | 68.0 {62-70} |
13.6 (14.6)d |
-0.01 (-0.29 to 0.26) | ||||
| SMD: standardized mean difference; Gen: general; Neur: neuraxial. | ||||||||
| a Mean Med (SD)[Range]{IQR}. | ||||||||
| b Arrow direction indicates better functional outcome. | ||||||||
| c Composite WOMAC includes pain, stiffness, and physical function. Physical function accounts for 68 of the 96 points. | ||||||||
| d Standard deviations derived from confidence intervals and appear small, but are consistent with reported statistical results. | ||||||||
Pooled
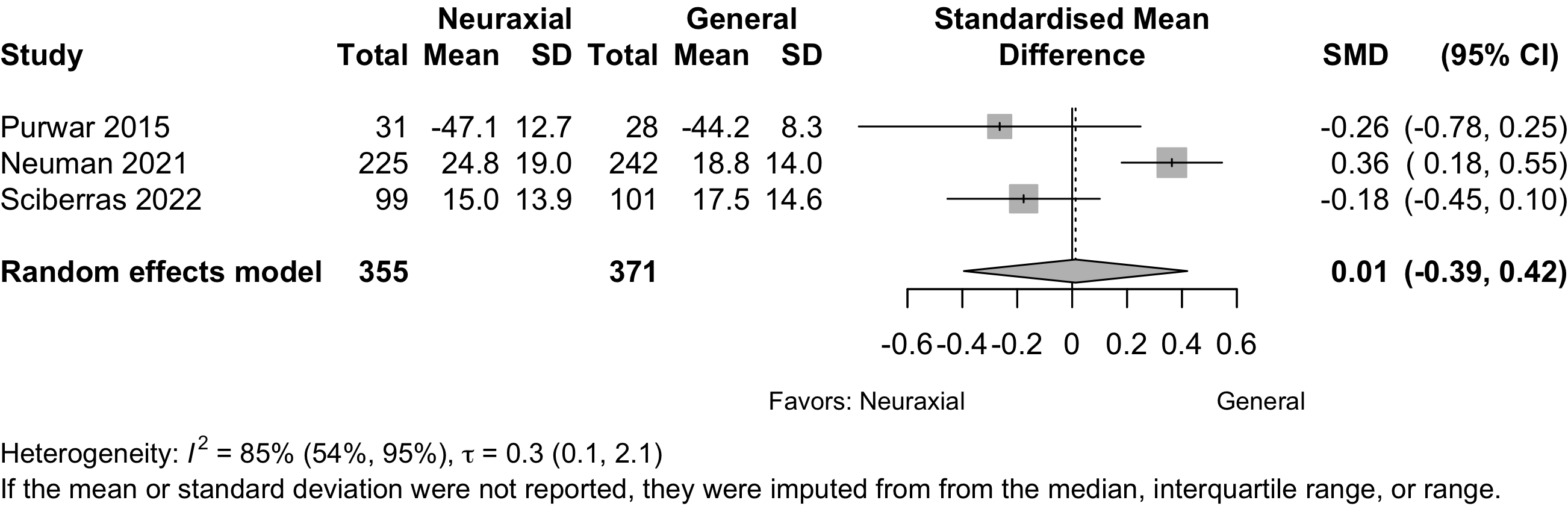
Using Neuman 2021 primary result from 1385 participants in a sensitivity analysis yield a pooled SMD -0.07 (95% CI, -0.25 to 0.12) and equivalent OR 0.89 (95% CI, 0.63–1.24).
Complications
| Study | N | Arm | Age | Surgery | N (%) | 0 – 100% | RD (95% CI) |
|---|---|---|---|---|---|---|---|
| MI | |||||||
| 164 | Gen | 83.0 [59-99] |
Ortho | 1 (0.6) | — | ||
| 158 | Neur | 82.9 [25-105] |
1 (0.6) | 0.0% (-1.7, 1.7) | |||
| 66 | Gen | 68.0 (11.0) |
Ortho | 2 (3.0) | — | ||
| 66 | Neur | 67.0 (12.0) |
1 (1.5) | -1.5% (-6.6, 3.6) | |||
| 66 | Neur | 66.0 (10.0) |
2 (3.0) | 0.0% (-5.8, 5.8) | |||
| 793 | Gen | 78.4 (10.6) |
Ortho | 9 (1.1) | — | ||
| 783 | Neur | 77.7 (10.7) |
6 (0.8) | -0.4% (-1.3, 0.6) | |||
| 471 | Gen | 77.0 {71-82} |
Ortho | 0 (0) | — | ||
| 471 | Neur | 77.0 {72-82} |
1 (0.2) | 0.2% (-0.4, 0.8) | |||
| 106 | Gen | 72.0 {69-76} |
Spine | 0 (0) | — | ||
| 111 | Neur | 73.0 {69-78} |
1 (0.9) | 0.9% (-1.6, 3.4) | |||
| Cardiac Arrest | |||||||
| 793 | Gen | 78.4 (10.6) |
Ortho | 0 (0) | — | ||
| 783 | Neur | 77.7 (10.7) |
2 (0.3) | 0.3% (-0.2, 0.7) | |||
| Other Cardiac | |||||||
| 18 | Gen | 67.7 (15.1) |
GI/Abd | 3 (16.7) | — | ||
| 18 | Neur | 64.9 (10.3) |
2 (11.1) | -5.6% (-28.1, 17.0) | |||
| 30 | Gen | 69.0 {62-74} |
Ortho | 2 (6.7) | — | ||
| 30 | Neur | 65.0 {62-68} |
0 (0) | -6.7% (-17.2, 3.9) | |||
| 164 | Gen | 83.0 [59-99] |
Ortho | 3 (1.8) | — | ||
| 158 | Neur | 82.9 [25-105] |
0 (0) | -1.8% (-4.2, 0.5) | |||
| 60 | Gen | 79.4 (7.7) |
Ortho | 3 (5.0) | — | ||
| 58 | Gen | 80.5 (6.7) |
2 (3.4) | -1.6% (-8.8, 5.7) | |||
| 58 | Neur | 81.6 (6.7) |
2 (3.4) | -1.6% (-8.8, 5.7) | |||
| 29 | Gen | 73.0 {72-74} |
Ortho | 1 (3.4) | — | ||
| 29 | Neur | 72.0 {70-73} |
3 (10.3) | 6.9% (-6.0, 19.8) | |||
Li 2022e,f |
471 | Gen | 77.0 {71-82} |
Ortho | 4 (0.8) | — | |
| 471 | Neur | 77.0 {72-82} |
3 (0.6) | -0.2% (-1.3, 0.9) | |||
| 20 | Gen | 62.6 (10.7) |
Other | 0 (0) | — | ||
| 20 | Neur | 65.5 (16.8) |
1 (5.0) | 5.0% (-7.8, 17.8) | |||
| 40 | Gen | 73.0 (6.0) |
Urol | 0 (0) | — | ||
| 40 | Neur | 71.0 (6.0) |
0 (0) | 0.0% (-4.8, 4.8) | |||
| 217 | Gen | 70.8 [61-84] |
Various | 2 (0.9) | — | ||
| 211 | Neur | 71.1 [61-84] |
3 (1.4) | 0.5% (-1.5, 2.5) | |||
| Stroke | |||||||
| 793 | Gen | 78.4 (10.6) |
Ortho | 7 (0.9) | — | ||
| 783 | Neur | 77.7 (10.7) |
5 (0.6) | -0.2% (-1.1, 0.6) | |||
| 471 | Gen | 77.0 {71-82} |
Ortho | 1 (0.2) | — | ||
| 471 | Neur | 77.0 {72-82} |
0 (0) | -0.2% (-0.8, 0.4) | |||
| 106 | Gen | 72.0 {69-76} |
Spine | 0 (0) | — | ||
| 111 | Neur | 73.0 {69-78} |
2 (1.8) | 1.8% (-1.2, 4.8) | |||
| AKI/Renal Failure | |||||||
| 164 | Gen | 83.0 [59-99] |
Ortho | 2 (1.2) | — | ||
| 158 | Neur | 82.9 [25-105] |
0 (0) | -1.2% (-3.3, 0.8) | |||
| 66 | Gen | 68.0 (11.0) |
Ortho | 1 (1.5) | — | ||
| 66 | Neur | 67.0 (12.0) |
0 (0) | -1.5% (-5.6, 2.6) | |||
| 66 | Neur | 66.0 (10.0) |
0 (0) | -1.5% (-5.6, 2.6) | |||
| 793 | Gen | 78.4 (10.6) |
Ortho | 55 (6.9) | — | ||
| 783 | Neur | 77.7 (10.7) |
32 (4.1) | -2.8% (-5.1, -0.6) | |||
| 106 | Gen | 72.0 {69-76} |
Spine | 0 (0) | — | ||
| 111 | Neur | 73.0 {69-78} |
1 (0.9) | 0.9% (-1.6, 3.4) | |||
| Pulmonary | |||||||
| 60 | Gen | 79.4 (7.7) |
Ortho | 4 (6.7) | — | ||
| 58 | Gen | 80.5 (6.7) |
5 (8.6) | 2.0% (-7.6, 11.5) | |||
| 58 | Neur | 81.6 (6.7) |
4 (6.9) | 0.2% (-8.8, 9.3)j,k | |||
| Pneumonia | |||||||
| 30 | Gen | 69.0 {62-74} |
Ortho | 1 (3.3) | — | ||
| 30 | Neur | 65.0 {62-68} |
0 (0) | -3.3% (-12.1, 5.4) | |||
| 164 | Gen | 83.0 [59-99] |
Ortho | 3 (1.8) | — | ||
| 158 | Neur | 82.9 [25-105] |
2 (1.3) | -0.6% (-3.3, 2.1) | |||
| 66 | Gen | 68.0 (11.0) |
Ortho | 1 (1.5) | — | ||
| 66 | Neur | 67.0 (12.0) |
0 (0) | -1.5% (-5.6, 2.6) | |||
| 66 | Neur | 66.0 (10.0) |
1 (1.5) | 0.0% (-4.2, 4.2) | |||
| 29 | Gen | 73.0 {72-74} |
Ortho | 4 (13.8) | — | ||
| 29 | Neur | 72.0 {70-73} |
1 (3.4) | -10.3% (-24.5, 3.9) | |||
| 793 | Gen | 78.4 (10.6) |
Ortho | 16 (2.0) | — | ||
| 783 | Neur | 77.7 (10.7) |
8 (1.0) | -1.0% (-2.2, 0.2) | |||
| 471 | Gen | 77.0 {71-82} |
Ortho | 1 (0.2) | — | ||
| 471 | Neur | 77.0 {72-82} |
0 (0) | -0.2% (-0.8, 0.4) | |||
| 106 | Gen | 72.0 {69-76} |
Spine | 0 (0) | — | ||
| 111 | Neur | 73.0 {69-78} |
2 (1.8) | 1.8% (-1.2, 4.8) | |||
| Pulmonary Congestion | |||||||
| 793 | Gen | 78.4 (10.6) |
Ortho | 8 (1.0) | — | ||
| 783 | Neur | 77.7 (10.7) |
9 (1.1) | 0.1% (-0.9, 1.2) | |||
| Pulmonary Embolism | |||||||
| 60 | Gen | 68.0 (7.0) |
Ortho | 1 (1.7) | — | ||
| 60 | Neur | 67.0 (7.0) |
1 (1.7) | 0.0% (-4.6, 4.6) | |||
| 164 | Gen | 83.0 [59-99] |
Ortho | 2 (1.2) | — | ||
| 158 | Neur | 82.9 [25-105] |
0 (0) | -1.2% (-3.3, 0.8) | |||
| 66 | Gen | 68.0 (11.0) |
Ortho | 2 (3.0) | — | ||
| 66 | Neur | 67.0 (12.0) |
0 (0) | -3.0% (-8.0, 2.0) | |||
| 66 | Neur | 66.0 (10.0) |
1 (1.5) | -1.5% (-6.6, 3.6) | |||
| 793 | Gen | 78.4 (10.6) |
Ortho | 5 (0.6) | — | ||
| 783 | Neur | 77.7 (10.7) |
4 (0.5) | -0.1% (-0.9, 0.6) | |||
| 106 | Gen | 72.0 {69-76} |
Spine | 1 (0.9) | — | ||
| 111 | Neur | 73.0 {69-78} |
1 (0.9) | -0.0% (-2.6, 2.5) | |||
| 217 | Gen | 70.8 [61-84] |
Various | 2 (0.9) | — | ||
| 211 | Neur | 71.1 [61-84] |
0 (0) | -0.9% (-2.5, 0.6) | |||
| Reintubation | |||||||
| 793 | Gen | 78.4 (10.6) |
Ortho | 7 (0.9) | — | ||
| 783 | Neur | 77.7 (10.7) |
4 (0.5) | -0.4% (-1.2, 0.4) | |||
| Gen: general anesthesia; Neur: neuraxial; RD: risk difference; Ortho: orthopedic; GI: gastrointestinal; Abd: abdominal; PE: pulmonary embolism; Ophtho: ophthalmologic; AKI: acute kidney injury. | |||||||
| a Bradycardia. | |||||||
| b Tachycardia. | |||||||
| c Arrhythmia. | |||||||
| d MI, heart failure, new onset arrhythmia. | |||||||
| e Bradycardia or tachycardia. | |||||||
| f Also reported hypo- (12.3% vs. 9.8%) or hypertension (3.8% vs. 12.8%), and left heart failure (0.9% vs. 0%). | |||||||
| g Unspecified adverse cardiac events. | |||||||
| h Renal failure | |||||||
| i AKI | |||||||
| j Verus combined general arms — RD 0.7% (-8.8 to 7.4), RR 0.90 (0.28–2.81). | |||||||
| k With general arms combined RR 0.90 (95% CI, 0.29–2.81). | |||||||
Pooled
Myocardial Infarction
Bradycardia
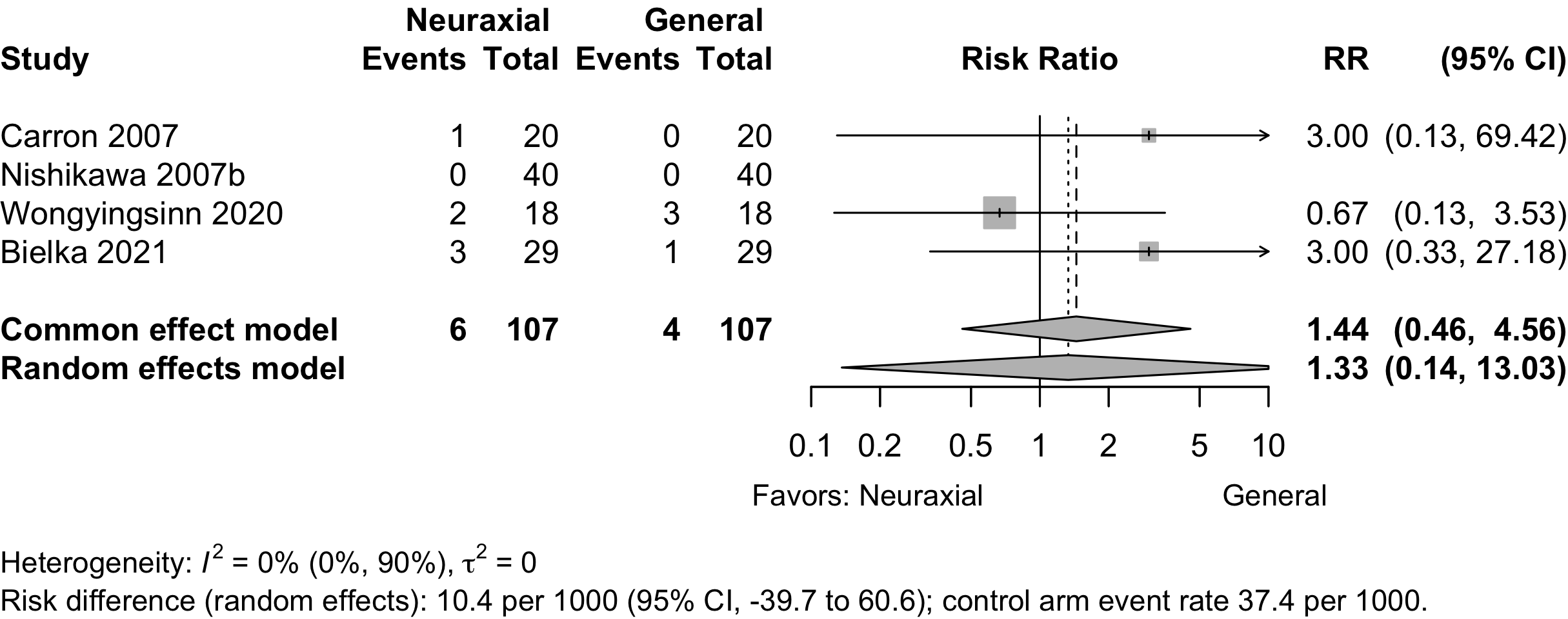
Prediction interval not displayed due to limited events.
Stroke
Acute Kidney Injury
Pneumonia
Pulmonary Embolism
Patient Satisfaction
| Study | N | Anesth | ASA | Agea | N (%) | 0 – 100% | RD (95% CI) |
|---|---|---|---|---|---|---|---|
| PS | |||||||
| Orthopedic | |||||||
| 60 | Gen | 123 | 68.0 (9.0) |
55 (91.7)b | — | ||
| 58 | Neur | 66.0 (7.8) |
45 (77.6)b | -14.1% (-26.9, -1.3) | |||
| 21 | Gen | 123 | 85.0 (5.0) |
15 (71.4)c | — | ||
| 19 | Neur | 83.0 (6.0) |
17 (89.5)c | 18.0% (-5.7, 41.8) | |||
| 80 | Gen | NR | 75.4 (5.6) |
69 (86.2)d | — | ||
| 160 | Neur | 75.6 (5.5) |
66 (82.5)d | 3.1% (-5.8, 12.1) | |||
| 661 | Gen | 1234 | 78.0 (11.0) |
564 (85.3)e | — | ||
| 647 | Neur | 78.0 (11.0) |
562 (86.9)e | 1.5% (-2.2, 5.3) | |||
| Urologic | |||||||
| 34 | Gen | NR | 66.0 (6.8) |
32 (94.1)b | — | ||
| 36 | Neur | 65.3 (6.9) |
35 (97.2)b | 3.1% (-6.5, 12.7) | |||
| 40 | Gen | 12 | 73.0 (6.0) |
32 (80.0)f | — | ||
| 40 | Neur | 71.0 (6.0) |
28 (70.0)f | -10.0% (-28.9, 8.9) | |||
| 30 | Gen | 23 | 70.0 (9.6) |
22 (73.3)g | — | ||
| 30 | Neur | 76.4 (11.8) |
25 (83.3)g | 10.0% (-10.7, 30.7) | |||
| Neurosurgical | |||||||
| 25 | Gen | 123 | 62.7 (14.3) |
24 (96.0)b | — | ||
| 25 | Neur | 67.0 (10.4) |
22 (88.0)b | -8.0% (-22.9, 6.9) | |||
| Vascular | |||||||
| 20 | Gen | 23 | 61.2 (10.5) |
12 (60.0)b | — | ||
| 20 | Neur | 60.6 (9.7) |
18 (90.0)b | 30.0% (4.8, 55.2) | |||
| Other | |||||||
| 20 | Gen | 123 | 62.6 (10.7) |
14 (70.0)b | — | ||
| 20 | Neur | 65.5 (16.8) |
18 (90.0)b | 20.0% (-4.0, 44.0) | |||
| Gen: general; Neur: neuraxial; Anesth: anesthetic; ASA PS: ASA Physical Status; RD: risk difference. | |||||||
| a Mean (SD). | |||||||
| b Satisfied. | |||||||
| c Excellent/good | |||||||
| d Not specified | |||||||
| e Satisfaction with all aspects of anesthesia care | |||||||
| f Very satisfied | |||||||
| g Very good | |||||||
Pooled
Length of Stay
| Study | N | Anesth | PSa | Ageb | LOSb | 0 – 20 days | Country |
|---|---|---|---|---|---|---|---|
| Orthopedic | |||||||
| 30 | Gen | 123 | 69.0 {62-74} |
9.0 {7-10} |
China | ||
| 30 | Neur | 123 | 65.0 {62-68} |
7.5 {6-11} |
|||
| 60 | Gen | 123 | 68.0 (7.0) |
3.0 [1-4] |
Sweden | ||
| 60 | Neur | 123 | 67.0 (7.0) |
3.0 [1-4] |
|||
| 164 | Gen | 1234 | 83.0 [59-99] |
15.9 (13.7) |
UK | ||
| 158 | Neur | 1234 | 82.9 [25-105] |
16.2 (14.6) |
|||
| 33 | Gen | 123 | 75.1 (6.1) |
8.2 |
Greece | ||
| 37 | Neur | 123 | 77.1 (6.5) |
8.2 |
|||
| 60 | Gen | NR | 79.4 (7.7) |
6.5 {5-9} |
South Korea | ||
| 58 | Gen | NR | 80.5 (6.7) |
7.0 {5-9} |
|||
| 58 | Neur | NR | 81.6 (6.7) |
7.0 {5-11} |
|||
| 80 | Gen | NR | 75.4 (5.6) |
4.3 (0.9) |
China | ||
| 80 | Neur | NR | 75.6 (5.5) |
4.1 (1.1) |
|||
| 80 | Neur | NR | 75.0 (5.2) |
4.2 (0.9) |
|||
| 211 | Gen | 6.0 {5-10} |
Canada | ||||
| 210 | Neur | 6.0 {4-9} |
|||||
| 593 | Gen | 3.0 {3-5} |
USA | ||||
| 585 | Neur | 3.0 {2-5} |
|||||
| 154 | Gen | 123 | 74.1 (4.2) |
9.2 (2.1) |
China | ||
| 127 | Neur | 123 | 73.1 (6.2) |
9.0 (2.1) |
|||
| 471 | Gen | 1234 | 77.0 {71-82} |
7.0 {6-10} |
China | ||
| 471 | Neur | 1234 | 77.0 {72-82} |
7.0 {5-10} |
|||
| Various | |||||||
| 217 | Gen | 1234 | 70.8 [61-84] |
8.0 [2-20] |
Denmark | ||
| 211 | Neur | 1234 | 71.1 [61-84] |
9.0 [2-21] |
|||
| Gastrointestinal/Abdominal | |||||||
| 116 | Gen | NR | 74.8 (4.0) |
13.2 (1.3) |
China | ||
| 117 | Neur | NR | 75.7 (4.2) |
9.0 (1.8) |
|||
| Other | |||||||
| 20 | Gen | 123 | 62.6 (10.7) |
9.1 (6.3) |
Italy | ||
| 20 | Neur | 123 | 65.5 (16.8) |
7.2 (3.4) |
|||
| Spine | |||||||
| 106 | Gen | NR | 72.0 {69-76} |
3.0 {2-3} |
USA | ||
| 111 | Neur | NR | 73.0 {69-78} |
3.0 {2-3} |
|||
| Anesth: anesthetic; NR: not reported. | |||||||
| a ASA Physical Status. | |||||||
| b Mean Med (SD)[Range]{IQR}. | |||||||
Pooled
Discharge Location
| Study | N | Arm | Agea | Country | Discharge to Institution | RR (95% CI) | |
|---|---|---|---|---|---|---|---|
| N (%) | 0 — 100% | ||||||
| Randomized Clinical Trial — Orthopedic | |||||||
| 777 | Gen | 78.4 (10.6) |
USA | 586 (75.4) | |||
| 777 | Neur | 77.7 (10.7) |
576 (74.1) | 0.98 (0.93-1.04) | |||
| 279 | Gen | USA | 233 (83.5) | ||||
| 292 | Neur | 208 (71.2) | 0.85 (0.78-0.93) | ||||
| 437 | Gen | USA | 297 (68.0) | ||||
| 431 | Neur | 297 (68.9) | 1.01 (0.93-1.11) | ||||
| Gen: general; Neur: neuraxial; RR: risk ratio. | |||||||
| a Mean Med (SD)[Range]{IQR}. | |||||||
Mortality
| Study | N | Arm | Surgery | ASA | Agea | Mortality | RD (95% CI) | |
|---|---|---|---|---|---|---|---|---|
| PS | N (%) | 0 - 100% | ||||||
| Hospital | ||||||||
| 217 | Gen | Various | 1234 | 70.8 [61-84] |
3 (1.4) | — | ||
| 211 | Neur | 71.1 [61-84] |
0 (0) | -1.4% (-3.2, 0.4) | ||||
| 60 | Gen | Ortho | 123 | 68.0 (7.0) |
0 (0) | — | ||
| 60 | Neur | 67.0 (7.0) |
0 (0) | 0.0% (-3.2, 3.2) | ||||
| 60 | Gen | Ortho | NR | 79.4 (7.7) |
1 (1.7) | — | ||
| 58 | Gen | 80.5 (6.7) |
0 (0) | -1.7% (-6.2, 2.9) | ||||
| 58 | Neur | 81.6 (6.7) |
2 (3.4) | 1.8% (-3.9, 7.5) | ||||
| 106 | Gen | Spine | NR | 72.0 {69-76} |
1 (0.9) | — | ||
| 111 | Neur | 73.0 {69-78} |
0 (0) | -0.9% (-3.5, 1.6) | ||||
| 790 | Gen | Ortho | 1234 | 78.4 (10.6) |
13 (1.6) | — | ||
| 782 | Neur | 77.7 (10.7) |
5 (0.6) | -1.0% (-2.1, 0.0) | ||||
| 30-day | ||||||||
| 164 | Gen | Ortho | 1234 | 83.0 [59-99] |
8 (4.9) | — | ||
| 158 | Neur | 82.9 [25-105] |
5 (3.2) | -1.7% (-6.0, 2.6) | ||||
| 60 | Gen | Ortho | 123 | 68.0 (9.0) |
0 (0) | — | ||
| 58 | Neur | 66.0 (7.8) |
0 (0) | 0.0% (-3.3, 3.3) | ||||
| 21 | Gen | Ortho | 123 | 85.0 (5.0) |
0 (0) | — | ||
| 19 | Neur | 83.0 (6.0) |
0 (0) | 0.0% (-9.3, 9.3) | ||||
| 60 | Gen | Ortho | NR | 79.4 (7.7) |
2 (3.3) | 1.7% (-3.9, 7.2) | ||
| 58 | Gen | 80.5 (6.7) |
1 (1.7) | 0.1% (-4.6, 4.7) | ||||
| 58 | Neur | 81.6 (6.7) |
1 (1.7) | 0.1% (-4.6, 4.7) | ||||
| 464 | Gen | Ortho | 1234 | 77.0 {71-82} |
4 (0.9) | — | ||
| 469 | Neur | 77.0 {72-82} |
8 (1.7) | 0.8% (-0.6, 2.3) | ||||
| 90-day | ||||||||
| 217 | Gen | Various | 1234 | 70.8 [61-84] |
1 (0.5) | -0.9% (-2.7, 0.9) | ||
| 211 | Neur | 71.1 [61-84] |
0 (0) | -1.4% (-3.2, 0.4) | ||||
| 164 | Gen | Ortho | 1234 | 83.0 [59-99] |
12 (7.3) | 2.4% (-2.7, 7.6) | ||
| 158 | Neur | 82.9 [25-105] |
12 (7.6) | 2.7% (-2.6, 8.0) | ||||
| 60 | Gen | Ortho | NR | 79.4 (7.7) |
3 (5.0) | 3.3% (-3.1, 9.7) | ||
| 58 | Gen | 80.5 (6.7) |
2 (3.4) | 1.8% (-3.9, 7.5) | ||||
| 58 | Neur | 81.6 (6.7) |
3 (5.2) | 3.5% (-3.1, 10.1) | ||||
| 1-year | ||||||||
| 164 | Gen | Ortho | 1234 | 83.0 [59-99] |
19 (11.6) | 6.7% (0.8, 12.6) | ||
| 158 | Neur | 82.9 [25-105] |
32 (20.3) | 15.4% (8.3, 22.5) | ||||
| ASA PS: American Society of Anesthesiologists Physical Status; RD: risk difference; GI: gastrointestinal; Abd: abdominal (includes hepatic); Various: more that one procedure category. | ||||||||
| a Mean Med (SD)[Range]{IQR}. | ||||||||
Pooled
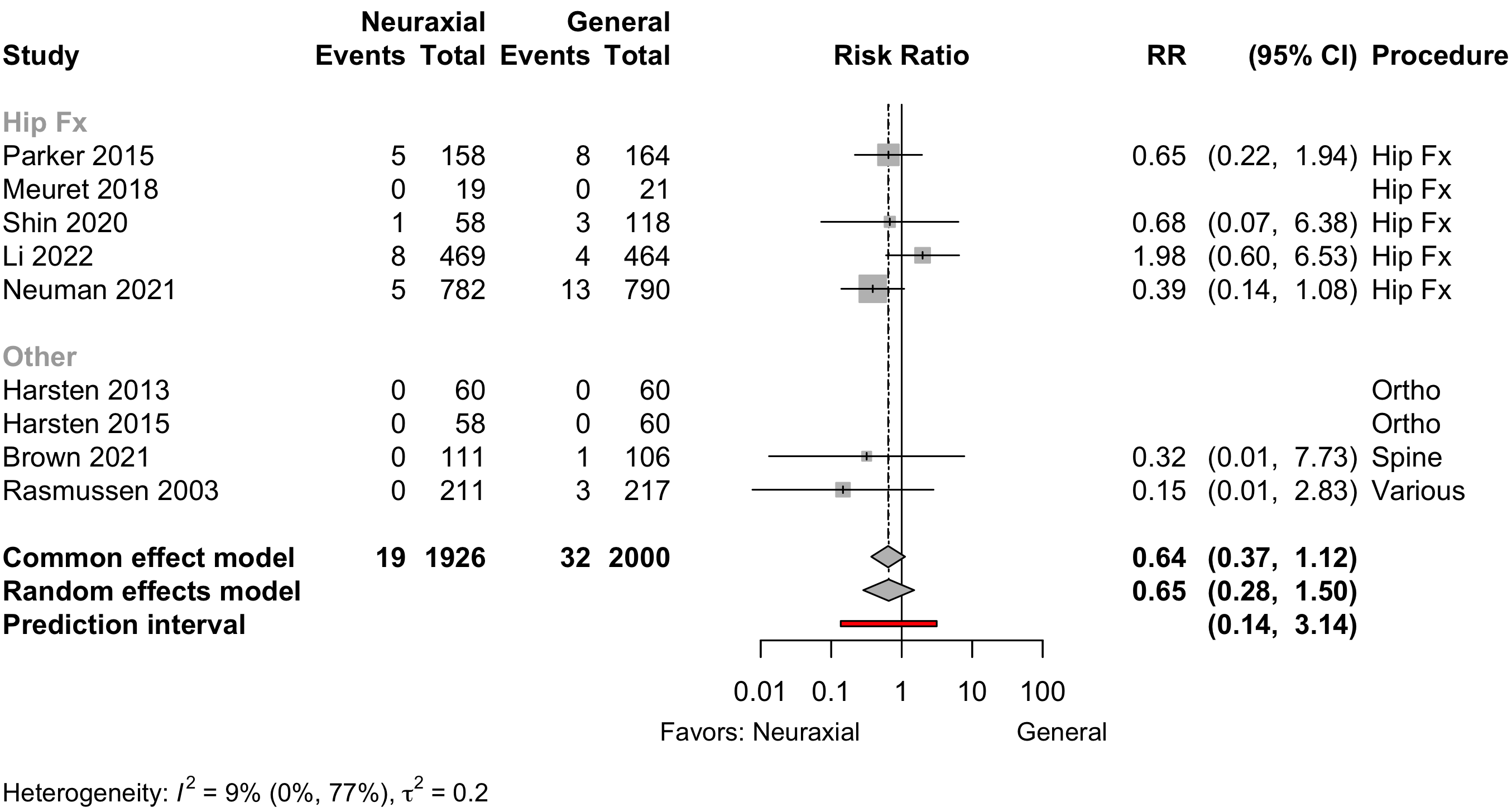
Other RR 0.20 (95% CI, 0.02–1.71)
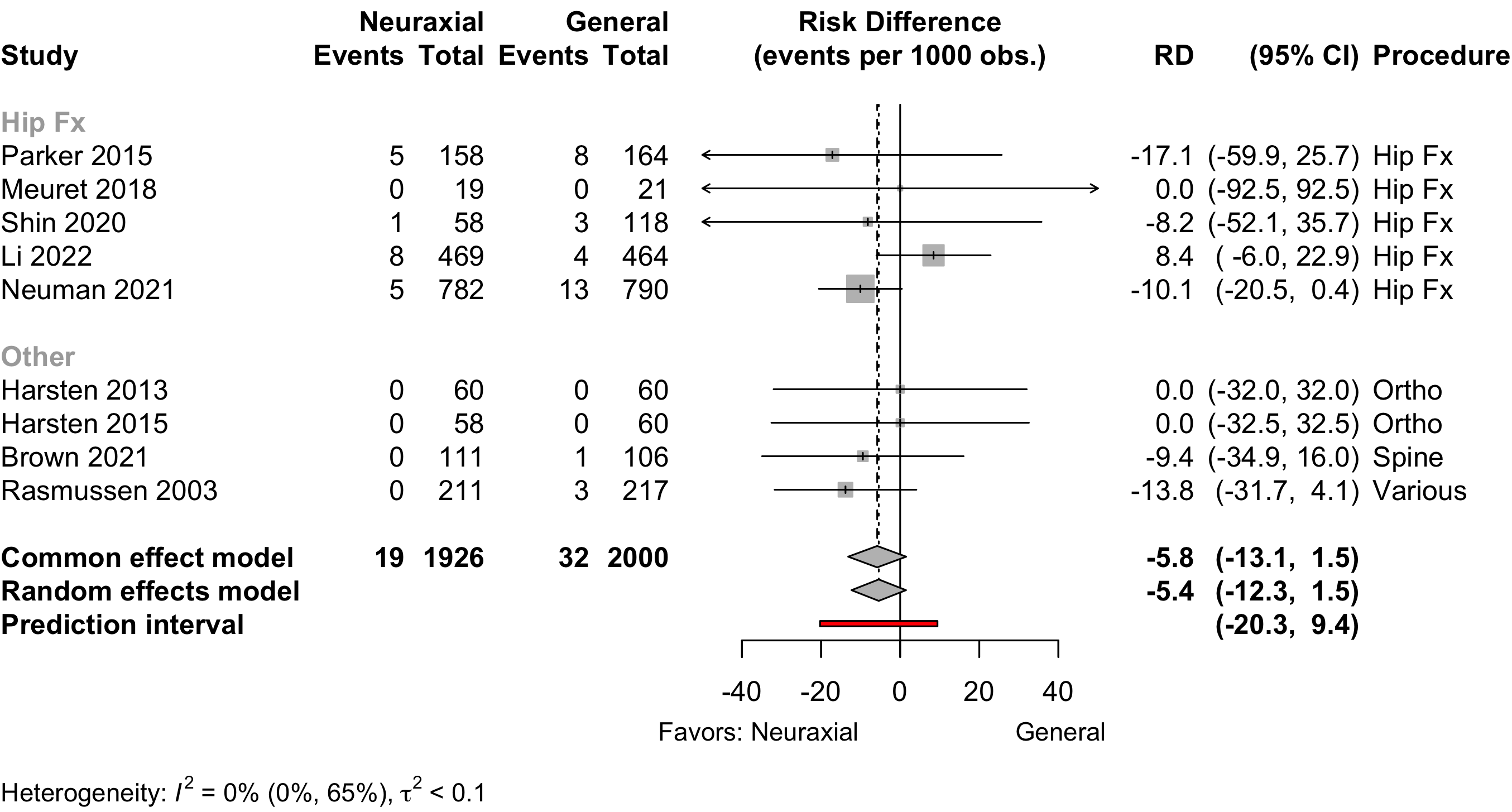
Hip fracture RD -3.6 (95% CI, -16.6 to 9.5)
Other RD -8.8 (95% CI, -21.1 to 3.6)
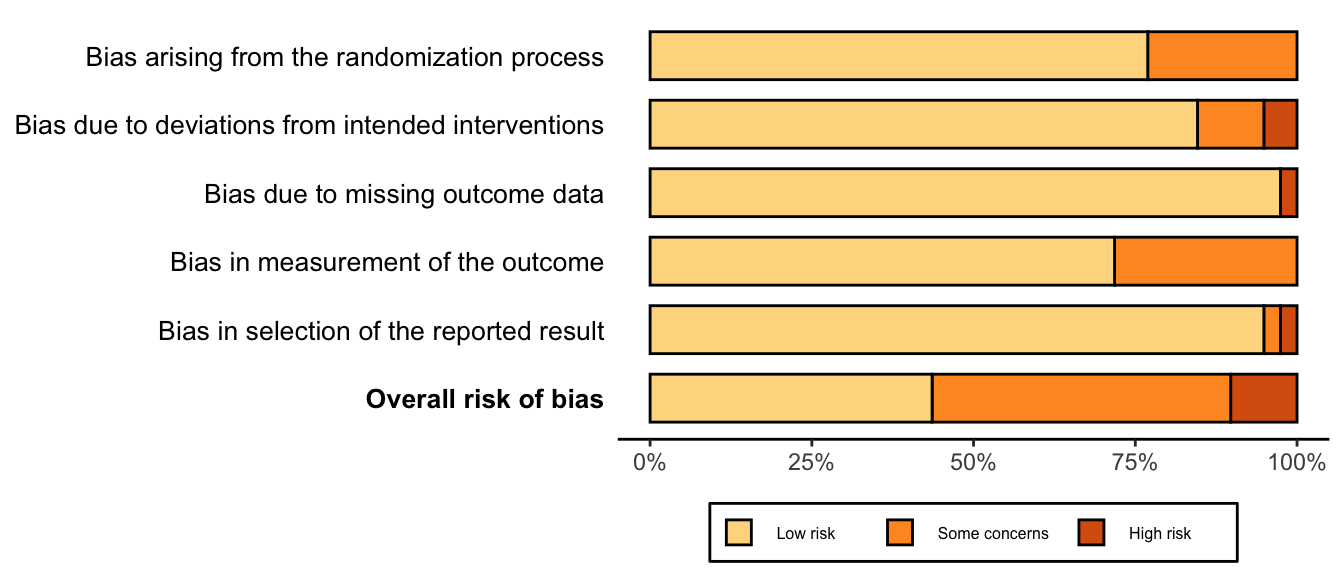
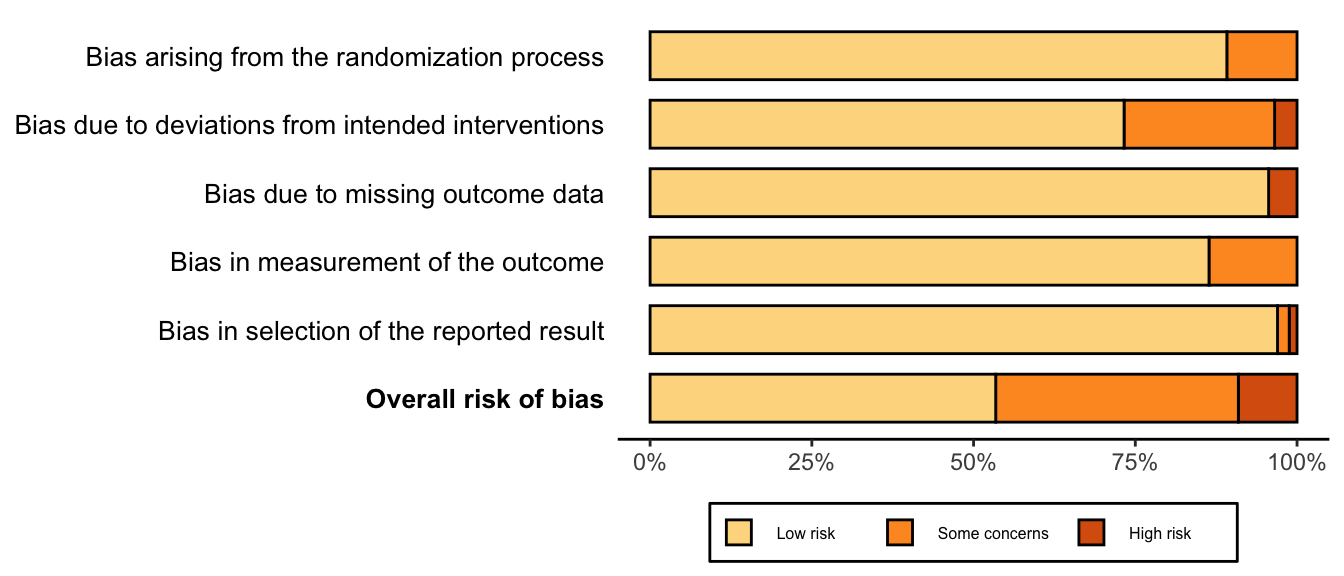
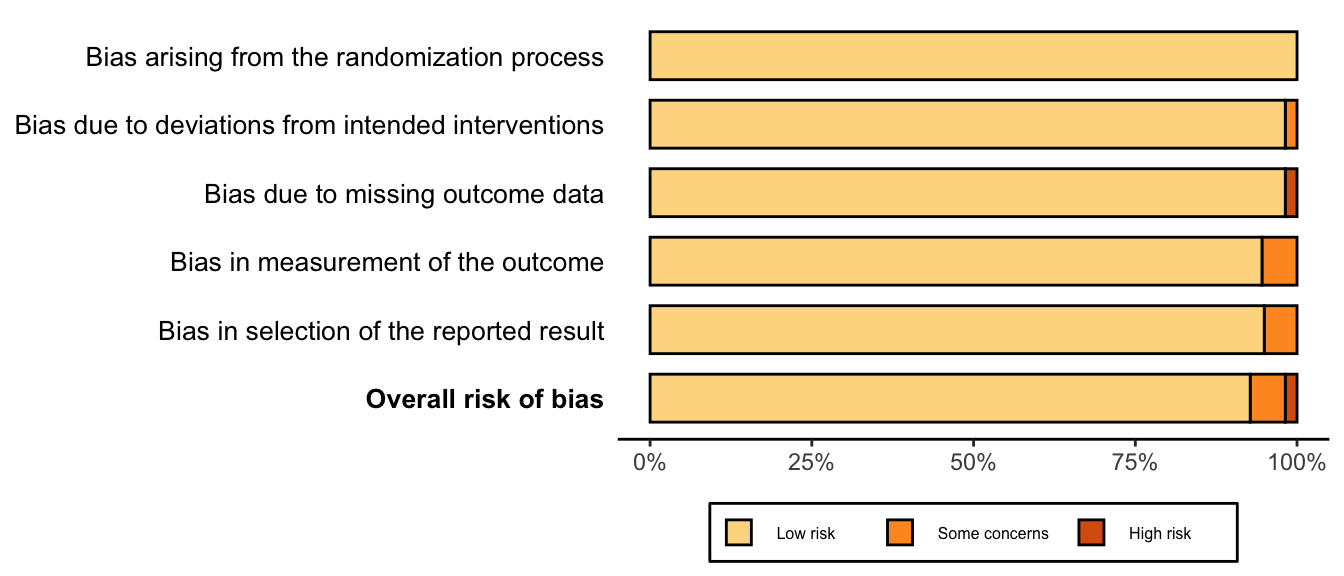
Risk of Bias